Nontraumatic thoracic aortic dissection
(Redirected from Thoracic Aortic Aneurysm)
Not to be confused with traumatic aortic transection
Background
- Most commonly seen in men 60-80 yrs old
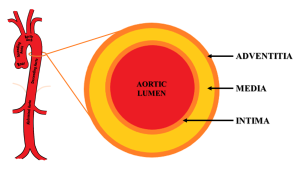
- Intimal tear with blood leaking into media
- Mortality in first 48 hours of acute presentation is high
- Diagnosis delayed > 24hr in 50% of cases
- Bimodal age distribution
- Young with risk factors
- Connective tissue disease (e.g. Marfan syndrome, Ehlers-Danlos, collagen vascular disease)
- Pregnancy, especially 3rd trimester
- Recent cardiac catheterization
- Bicuspid aortic valve
- Aortic coarctation
- Elderly males with chronic hypertension
- Atherosclerotic risk factors (smoking, hypertension, HLD, DM)
- Young with risk factors
Clinical Features
General
- Symptoms
- Tearing/ripping pain (10.8x increased disease probability)
- 64% described the pain as sharp vs 50.6% who described it as tearing or ripping[3]
- Migrating pain (7.6x)
- Sudden chest pain (2.6x)
- History of hypertension (1.5x)
- Tearing/ripping pain (10.8x increased disease probability)
- Signs
- Focal neurologic deficit (33x)
- Diastolic heart murmur (acute aortic regurg) (4.9x)
- Pulse deficit (2.7x)
- Hypertension at time of presentation (49% of all cases[4])
Specific
- Ascending Aorta
- Acute aortic regurgitation, leading to a diastolic decrescendo murmur, hypotension, or heart failure, in 50%-66%
- MI/Ischemia on ECG, usually inferior (dissection affects the right coronary artery more often than the left coronary artery[5])
- Cardiac Tamponade
- Hemothorax - if adventitia disruption
- Horners, partial - sympathetic ganglion
- Voice hoarseness - recurrent laryngeal nerve compression
- CVA/Syncope - if carotid extension
- Neurological deficits
- SBP>20mmhg difference between arms
- Hypertension at time of presentation (35.7% of all cases[4])
- Descending Aorta
- Chest pain, back pain, abdominal pain
- Pain abrupt, severe (90% of patients) radiating to back
- Hypertension at time of presentation (70.1% of all cases[4])
- Hemiplegia, neuropathy (15%)
- Renal failure
- Distal Pulse deficits/ limb ischemia
- Mesenteric ischemia
- Chest pain, back pain, abdominal pain
Differential Diagnosis
Chest pain
Critical
- Acute coronary syndromes (ACS)
- Aortic dissection
- Cardiac tamponade
- Coronary artery dissection
- Esophageal perforation (Boerhhaave's syndrome)
- Pulmonary embolism
- Tension pneumothorax
Emergent
- Cholecystitis
- Cocaine-associated chest pain
- Mediastinitis
- Myocardial rupture
- Myocarditis
- Pancreatitis
- Pericarditis
- Pneumothorax
Nonemergent
- Aortic stenosis
- Arthritis
- Asthma exacerbation
- Biliary colic
- Costochondritis
- Esophageal spasm
- Gastroesophageal reflux disease
- Herpes zoster / Postherpetic Neuralgia
- Hypertrophic cardiomyopathy
- Hyperventilation
- Mitral valve prolapse
- Panic attack
- Peptic ulcer disease
- Pleuritis
- Pneumomediastinum
- Pneumonia
- Rib fracture
- Stable angina
- Thoracic outlet syndrome
- Valvular heart disease
- Muscle sprain
- Psychologic / Somatic Chest Pain
- Spinal Root Compression
- Tumor
Hypertension
- Hypertensive emergency
- Stroke
- Sympathetic crashing acute pulmonary edema
- Ischemic stroke
- Intracranial hemorrhage
- Preeclampsia/Eclampsia
- Autonomic dysreflexia
- Scleroderma renal crisis
- Acute glomerulonephritis
- Type- I myocardial infarction
- Volume overload
- Urinary obstruction
- Drug use or overdose (e.g stimulants, especially alcohol, cocaine, or Synthroid)
- Renal Artery Stenosis
- Nephritic and nephrotic syndrome
- Polycystic kidney disease
- Tyramine reaction
- Cushing's syndrome
- Obstructive sleep apnea
- Pheochromocytoma
- Hyperaldosteronism
- Hyperthyroidism
- Anxiety
- Pain
- Oral contraceptive use
Evaluation
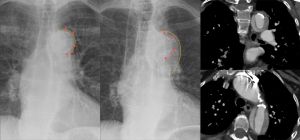
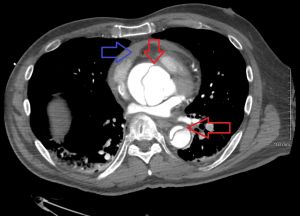
Dissection of the aortic arch: initial CXR normal visualization of the calcification shadow in the aortic arch (left); CXR 4 months later with calcification shifted centrally into the shadow of the aortic arch with a blurred external border (middle); CT scan coronal (top right) and axial (lower right).
Aortic Dissection Detection Risk Score (ADD-RS)
A score 1 should be awarded for each of the 3 categories that contain at least one of the listed features
| Predisposing conditions | Pain features | Physical findings |
|
Chest, back, or abdominal pain described as:
AND
|
|
| Score | Category | Prevalence |
| 0 | Low | 6% |
| 1 | Intermediate | 27% |
| >1 | High | 39% |
No Risk Factor Screening
- CXR
- Abnormal in 90% (3.4x)
- Mediastinal widening (seen in 56-63%)
- Left sided pleural effusion (seen in 19%)
- Widening of aortic contour (seen in 48%), displaced calcification (6mm), Calcium sign (look for white line of calcium within aortic knob and measure to outer edge of the aortic knob - distance greater than 0.5 cm is positive and > 1 cm is highly suspicious for dissection), aortic kinking, double density sign
Low-Intermediate
- D-dimer for ADD-RS ≤ 1 (low or intermediate risk)
High Risk/Definitive
- CT aortogram chest
- Study of choice
- Similar sensitivity/specificity to TEE and MRA
- TEE
- If CT delayed due to contrast allergy or availability, or patient instability.
- TEE has a sensitivity of 98% and 95% specific[9]
Other Findings

Type A Aortic Dissection[10]
- ECG
- LVH on admission ECG (3.2x)
- Ischemia (esp inferior) - 15%
- Nonspec ST-T changes - 40%
- Bedside US
- Can help in ruling in patients when AOFT is >4cm
- Rule out pericardial effusion and tamponade, especially in hypotension, syncope, dyspnea
Aortic Dissection Classification
- Stanford
- Type A: Involves any portion of ascending aorta
- Type B: Isolated to descending aorta
- De Bakey
- Type I: Involves the ascending and descending aorta
- Type II: Involves only the ascending aorta
- Type III: Involves only the descending aorta
| Image | 
|

|

|
| Percentage | 60% | 10–15% | 25–30% |
| Type | DeBakey I | DeBakey II | DeBakey III |
| Classification | Stanford A (Proximal) | Stanford B (Distal) | |
Management
General Principles
- Control pain to reduce sympathetic stimulation.
- Fentanyl is easily titratable with minimal cardiovascular effects
- Right radial arterial line or right arm blood pressure will generally be the most accurate
- Reducing heart rate while maintaining low-normal blood pressure reduces aortic flow acceleration, thereby reducing shear force on the intimal wall
- Goal: HR < 60 bpm, SBP 100-120 mmHg
- Control heart rate before blood pressure[11]
- Beta blockers are good first-line option, since they reduce heart rate and aortic wall tension
- Use β-blockers with caution in severe, acute aortic regurgitation - may worsen shock if dependent on compensatory tachycardia
Heart Rate control
- Esmolol
- Advantage of short half life, easily titratable
- Bolus 0.5mg/kg over 1min; infuse 0.05mg/kg/min (titrate upward in 0.05mg/kg/min increments to a maximum of 0.3 mg/kg/min)
- Esmolol Drip Sheet
- Labetalol - has both α and beta effects
- Push dose - 10-20mg with repeat doses of 20-40mg q10min up to 300mg
- Drip - Load 15-20mg IV, followed by 5mg/hr
- Metoprolol
- 5mg IV x 3; infuse at 2-5mg/hr
- Diltiazem - Use if contraindications to beta-blockers
- Loading 0.25mg/kg over 2–5 min, followed by a drip of 5mg/h
Blood pressure control (vasodilators)
Use if needed after beta-blockade.
- Nicardipine:
- 5mg/hr start, then titrate up by 2.5mg/hr every 10 min until goal
- Once at goal, drop to 3mg/hr and re-titrate from there
- May initially bolus 2mg IV[12]
- Clevidipine
- 1-2 mg/hr
- Double dose every 90 seconds until approaching goal BP, then increase in smaller amounts every 5-10 minutes until goal achieved.[13]
- Nitroprusside 0.3-0.5mcg/kg/min - Risk of cerebral blood vessel vasodilation and CN/Thiocynate toxicity
- Fenoldopam
- Enalapril
Surgery
- Type A (any portion of ascending aorta)
- Requires surgery
- Type B (isolated to descending aorta)
- Primarily medical management with surgery consultation
Disposition
- Admission to OR or ICU
Complications
- AV Regurgitation/Insufficiency
- CHF with diastolic murmur
- Rupture
- Pericardium: cardiac tamponade
- Mediastinum: hemothorax
- Vascular obstruction
See Also
External Links
- NNT Aortic Dissection LRs
- AHA Full Guidelines
- AHA Quick Summary
- ALiEM Paucis Verbis: International Registry on Aortic Dissection (IRAD)
- MDcalc ADD Score
References
- ↑ Hirst AE Jr, et al. Dissecting aneurysm of the aorta: a review of 505 cases. Medicine (Baltimore). 1958;37(3):217-279.
- ↑ Harris, KM. et al. Early mortality in type A acute aortic dissection: Insights from the International Registry of Acute Aortic Dissection. JAMA Cardiol. 2022;7(10):1009-1015.
- ↑ Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897–903.
- ↑ 4.0 4.1 4.2 Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000; 283(7):897-903.
- ↑ Spittell PC, S et al. Clinical features and differential diagnosis of aortic dissection: experience with 236 cases (1980 through 1990) Mayo Clin Proc. 1993;68:642–51.
- ↑ Circulation. 2018 Jan 16;137(3):250-258. doi: 10.1161/CIRCULATIONAHA.117.029457. Epub 2017 Oct 13. Nazerian, et al. Diagnostic Accuracy of the Aortic Dissection Detection Risk Score Plus D-Dimer for Acute Aortic Syndromes: The ADvISED Prospective Multicenter Study.
- ↑ Asha SE et al. "A systematic review and meta-analysis of D-dimer as a rule out test for suspected acute aortic dissection." Annals of EM. 66;4;368-377Ocotber 2015.
- ↑ Shimony A, et al. Meta-analysis of usefulness of d-dimer to diagnose acute aortic dissection. Am J Cardiol. 2011; 107(8):1227-1234.
- ↑ Shiga T, Wajima Z, Apfel CC, Inoue T, Ohe Y. Diagnostic accuracy of transesophageal echocardiography, helical computed tomography, and magnetic resonance imaging for suspected thoracic aortic dissection: systematic review and meta-analysis. Arch Intern Med. 2006 Jul 10;166(13):1350-6.
- ↑ http://www.thepocusatlas.com/echocardiography-1
- ↑ Tsai TT, Nienaber CA, and Eagle KA. Acute Aortic Syndromes. Circulation. 2005;112:3802–3813
- ↑ Curran MP et al. Intravenous Nicardipine. Drugs 2006; 66(13): 1755-1782. http://emcrit.org/wp-content/uploads/2014/07/bolus-dose-nicardipine.pdf
- ↑ UpToDate Inc. Clevidipine [Drug information]. In:UpToDate Lexidrug. Wolters Kluwer; 2025. Accessed August 1, 2025.