Ischemic stroke
Background
Ischemic stroke causes (87%)
- Thrombotic (80% of ischemic CVA)
- Atherosclerosis
- Vasculitis
- Vertebral and carotid artery dissection
- Often preceded by yoga, spinal manipulation, coughing, vomiting
- Polycythemia
- Hypercoagulable state (oral contraceptives, antiphospholipid antibodies, protein S and C deficiencies, sickle cell anemia)
- Infection
- Toxicologic exposure (cocaine, amphetamines, etc.)
- Embolic (20% of ischemic CVA)
- Valvular vegetations
- Mural thrombi
- Arterial-arterial emboli from proximal source (ex. amaurosis fugax -> emboli from a proximal carotid artery plaque embolizes to the ophthalmic artery, causing transient monocular blindness)
- Fat emboli
- Septic emboli
- Hypoperfusion
- Cardiac failure resulting in systemic hypotension
- Cryptogenic
- Cryptogenic Stroke (CS) is defined as an Ischemic stroke of obscure or unknown origin. Its causes are unknown. It is transitory or reversible.[1]
Clinical Features
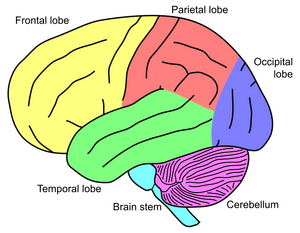
Anterior Circulation
Internal Carotid Artery
- Tonic gaze deviation towards lesion
- Global aphasia, dysgraphia, dyslexia, dyscalculia, disorientation (dominant lesion)
- Spatial or visual neglect (non-dominant lesion)
Anterior Cerebral Artery (ACA)
Signs and Symptoms:
- Contralateral sensory and motor symptoms in the lower extremity (sparing hands/face)
- Urinary and bowel incontinence
- Left sided lesion: akinetic mutism, transcortical motor aphasia
- Right sided lesion: Confusion, motor hemineglect
- Presence of primitive grasp and suck reflexes
- May manifest gait apraxia
Middle Cerebral Artery (MCA)

Patient with stroke (forehead sparing).
Signs and Symptoms:
- Hemiparesis, facial plegia, sensory loss contralateral to affected cortex
- Motor deficits found more commonly in face and upper extremity than lower extremity
- Dominant hemisphere involved: aphasia
- Wernicke's aphasia (receptive aphasia) -> patient unable to process sensory input and does not understand verbal communication
- Broca's aphasia (expressive aphasia) -> patient unable to communicate verbally, even though understanding may be intact
- Nondominant hemisphere involved: dysarthria (motor deficit of the mouth and speech muscles; understanding intact) w/o aphasia, inattention and neglect side opposite to infarct
- Contralateral homonymous hemianopsia
- Gaze preference toward side of infarct
- Agnosia (inability to recognize previously known subjects)
Posterior circulation
- Blood supply via the vertebral artery
- Branches include, AICA, Basilar artery, PCA and PICA
Signs and Symptoms:
- Crossed neuro deficits (i.e., ipsilateral CN deficits w/ contralateral motor weakness)
- Multiple, simultaneous complaints are the rule (including loss of consciousness, nausea/vomiting, alexia, visual agnosia)
- 5 Ds: Dizziness (Vertigo), Dysarthria, Dystaxia, Diplopia, Dysphagia
- Isolated events are not attributable to vertebral occlusive disease (e.g. isolated lightheadedness, vertigo, transient ALOC, drop attacks)
- Approximately 25% associated with aortic dissection
Basilar artery
Signs and Symptoms:
- Quadriplegia, coma, locked-in syndrome
- "Crossed signs" in which a patient has unilateral cranial nerve deficits but contralateral hemiparesis and hemisensory loss suggest brainstem infarction
- Sparing of vertical eye movements (CN III exits brainstem just above lesion)
- Thus, may also have miosis b/l
- One and a half syndrome (seen in a variety of brainstem infarctions)
- "Half" - INO (internuclear ophthalmoplegia) in one direction
- "One" - inability for conjugate gaze in other direction
- Convergence and vertical EOM intact
- Medial inferior pontine syndrome (paramedian basilar artery branch)
- Medial midpontine syndrome (paramedian midbasilar artery branch)
- Medial superior pontine syndrome (paramedian upper basilar artery branches)
Superior Cerebellar Artery (SCA)
- ~2% of all cerebral infarctions[2]
- May present with nonspecific symptoms - nausea/vomiting, dizziness, ataxia, nystagmus (more commonly horizontal)[3]
- Lateral superior pontine syndrome
- Ipsilateral ataxia, nausea/vomiting, nystagmus, Horner syndrome, conjugate gaze paresis
- Contralateral loss of pain/temperature in face/extremities/trunk, and loss of proprioception/vibration in LE > UE
Posterior Cerebral Artery (PCA)
Signs and Symptoms:
- Common after CPR, as occipital cortex is a watershed area
- Unilateral headache (most common presenting complaint)
- Visual field defects (contralateral homonymous hemianopsia, unilateral blindness)
- Visual agnosia - can't recognize objects
- Possible macular sparing if MCA unaffected
- Motor function is typically minimally affected
- Lateral midbrain syndrome (penetrating arteries from PCA)
- Medial midbrain syndrome (upper basilar and proximal PCA)
Anterior Inferior Cerebellar Artery (AICA)
- Lateral inferior pontine syndrome
- Ipsilateral facial paralysis, loss of corneal reflex (CN VII)
- Ipsilateral loss of pain/temperature (CN V)
- Nystagmus, nausea/vomiting, vertigo, ipsilateral hearing loss (CN VIII)
- Ipsilateral limb and gait ataxia
- Ipsilateral Horner syndrome
- Contralateral loss of pain/temperature in trunk and extremities (lateral spinothalamic)
Posterior Inferior Cerebellar Artery (PICA)
Signs and Symptoms:
- Lateral medullary/Wallenberg syndrome
- Ipsilateral cerebellar signs, ipsilateral loss of pain/temperature of face, ipsilateral Horner syndrome, ipsilateral dysphagia and hoarseness, dysarthria, vertigo/nystagmus
- Contralateral loss of pain/temp over body
- Also caused by vertebral artery occlusion (most cases)
Internal Capsule and Lacunar Infarcts
- May present with either lacunar c/l pure motor or c/l pure sensory (of face and body)[4]
- Pure c/l motor - posterior limb of internal capsule infarct
- Pure c/l sensory - thalamic infarct (Dejerine and Roussy syndrome)
- C/l motor plus sensory if large enough
- Clinically to cortical large ACA + MCA stroke - the following signs suggest cortical rather than internal capsule[5]:
- Gaze preference
- Visual field defects
- Aphasia (dominant lesion, MCA)
- Spatial neglect (non-dominant lesion)
- Others
- Ipsilateral ataxic hemiparesis, with legs worse than arms - posterior limb of internal capsule infarct
- Dysarthria/Clumsy Hand Syndrome - basilar pons or anterior limb of internal capsule infarct
Anterior Spinal Artery (ASA)
Superior ASA
- Medial medullary syndrome - displays alternating pattern of sidedness of symptoms below
- Contralateral arm/leg weakness and proprioception/vibration
- Tongue deviation towards lesion
Inferior ASA
- ASA syndrome
- Watershed area of hypoperfusion in T4-T8
- Bilateral pain/temp loss in trunk and extremities (spinothalamic)
- Bilateral weakness in trunk and extremities (corticospinal)
- Preservation of dorsal columns
Differential Diagnosis
Stroke-like Symptoms
- Stroke
- Seizures/postictal paralysis (Todd paralysis)
- Syncope
- Subdural hemorrhage
- Epidural hemorrhage
- Hypoglycemia
- Hyponatremia
- Meningitis/encephalitis
- Hyperosmotic Coma
- Labyrinthitis
- Drug toxicity
- Bell's Palsy
- Complicated migraine
- Meniere Disease
- Demyelinating disease (MS)
- Conversion disorder
- Transient global amnesia
- Giant cell arteritis
- Cerebral sinus thrombosis
Evaluation
Stroke Work-Up
- Labs
- POC glucose
- CBC
- Chemistry
- Coags
- Troponin
- T&S
- ECG
- In large ICH or stroke, may see deep TWI and prolong QT, occ ST changes
- Head CT (non-contrast)
- Also consider:
MR Imaging (for Rule-Out CVA or TIA)
- MRI Brain with DWI, ADC (without contrast) AND
- Cervical vascular imaging (ACEP Level B in patients with high short-term risk for stroke):[9]
- MRA brain (without contrast) AND
- MRA neck (without contrast)
- May instead use Carotid CTA or US (Carotid US slightly less sensitive than MRA)[10] (ACEP Level C)
Management
To differentiate between tPA and non-tPA candidates see Thrombolysis in Acute Ischemic Stroke (tPA)
Both tPA AND non-tPA candidates
- Prevent dehydration
- Maintain SpO2 > 92%
- Maintain blood glucose between 140 and 180 mg/dL
- Prevent fever
- HOB > 30°
tPA Candidate
- tPA
- Hypertension
- Lower SBP to < 185, DBP to < 110
- Goal MAP < 130
- Options:
- Labetalol 10–20 mg IV over 1–2 min; may repeat x1 OR
- Nitroglycerin paste, 1–2 in. to skin OR
- Nicardipine 5 mg/hr, titrate up by 2.5 mg/hr at 5-15 min intervals; max dose 15 mg/hr
- When desired blood pressure attained reduce to 3 mg/hr
Non-tPA Candidate
- Hypertension
- Allow permissive hypertension
- If SBP > 220 or DBP > 120, lower by 25% over 24 hrs (drug of choice is nicardipine)[11]
- Goal MAP for non-thrombolyzed, MAP < 150, per AHA guidelines[12]
- Aspirin 325mg (within 24-48hr)
- Clopidogrel 600 mg load (followed by 75 mg daily for 30-90 days)
- Anticoagulation not recommended for acute stroke (even for A-fib)
Endovascular Therapy
- Mechanical clot removal for large vessel occlusions (e.g. M1 occlusion, basilar artery occlusion)
- Early trials MR RESCUE, SYNTHESIS, and IMSIII showed no benefit and potential harm
- MR CLEAN Trial show promising outcomes[15]
- Participants had proximal intracranial artery occlusions
- Intervention was conducted within 6 hrs
- Functional independence of 32.6% with endovascular treatment and 19.1% with typical therapy
- AHA guidelines say the following patients are eligible for mechanical thrombectomy:
- 0-6 hours: pre-stroke mRS 01, ICA or M1 occlusion, age > 18, NIHSS > 5, puncture < 6 hours
- 0-6 hours: May also be reasonable in carefully selected patients with M2 or M3 occlusions
- 6-16 hours: anterior circulation LVO who meet DAWN or DEFUSE 3 criteria
- 16-24 hours: anterior circulation LVO who meet DAWN criteria
- May require careful patient selection based on last known normal, ICA/prox MCA occlusion, and additional diagnostic studies such as CT perfusion study, Rapid MRI, etc[16]
- Goal SBP <160 after endovascular therapy [17]
Cerebellar
- Early neurosurgical consultation is needed (herniation may lead to rapid deterioration)
- See Cerebellar Stroke
Corticosteroids
- Cochrane review showed no benefit in mortality or functional outcomes[18]
Disposition
- Admit all acute and subacute ischemic strokes
See Also
- Transient Ischemic Attack (TIA)
- Thrombolysis in Acute Ischemic Stroke (tPA)
- CVA (Post-tPA Hemorrhage)
- Intracerebral Hemorrhage
- Subarachnoid Hemorrhage (SAH)
- Cervical Artery Dissection
- NIH Stroke Scale
- Cerebellar Stroke
- Stroke (main)
- Alteplase
External Links
References
- ↑ [Finsterer J. Management of cryptogenic stroke. Acta Neurol Belg. 2010 Jun;110(2):135-47. PMID: 20873443].
- ↑ Macdonell RA, Kalnins RM, Donnan GA. Cerebellar infarction: natural history, prognosis, and pathology. Stroke. 18 (5): 849-55.
- ↑ Lee H, Kim HA. Nystagmus in SCA territory cerebellar infarction: pattern and a possible mechanism. J Neurol Neurosurg Psychiatry. 2013 Apr;84(4):446-51.
- ↑ Rezaee A and Jones J et al. Lacunar stroke syndrome. Radiopaedia. http://radiopaedia.org/articles/lacunar-stroke-syndrome.
- ↑ Internal Capsule Stroke. Stanford Medicine Guide. http://stanfordmedicine25.stanford.edu/the25/ics.html
- ↑ Mullins ME, Schaefer PW, Sorensen AG, Halpern EF, Ay H, He J, Koroshetz WJ, Gonzalez RG. CT and conventional and diffusion-weighted MR imaging in acute stroke: study in 691 patients at presentation to the emergency department. Radiology. 2002 Aug;224(2):353-60.
- ↑ Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006; 354(4):387–396.
- ↑ Douglas VC, Johnston CM, Elkins J, et al. Head computed tomography findings predict short-term stroke risk after transient ischemic attack. Stroke. 2003;34:2894-2899.
- ↑ ACEP Clinical Policy: Suspected Transient Ischemic Attack full text
- ↑ Nederkoorn PJ, Mali WP, Eikelboom BC, et al. Preoperative diagnosis of carotid artery stenosis. Accuracy of noninvasive testing. Stroke. 2002;33:2003-2008.
- ↑ Zha AM, et al. Recommendations for management of large hemispheric infarction. Curr Opin Crit Care. 2015; 21(2):91-8.
- ↑ Anton Helman. Emergency Medicine Cases. Episode 17 Part 1: Emergency Stroke Controversies. September 2011. https://emergencymedicinecases.com/episode-17-part-1-emergency-stroke-controversies/
- ↑ Journal Watch May 17, 2018 Clopidogrel plus Aspirin Has Benefits for TIA or Minor Stroke
- ↑ Clopidogrel and Aspirin in Acute Ischemic Stroke and High-Risk TIA N Engl J Med 2018; 379:215-225
- ↑ Berkhemer OA, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. NEJM. 2015; 372(1):11-20.
- ↑ Thrombectomy For Stroke At 6 To 16 Hours With Selection By Perfusion Imaging Albers, G.W., et al, N Engl J Med 378(8):708, February 22, 2018
- ↑ Smith M, Reddy U, Robba C, et al. Acute ischaemic stroke: challenges for the intensivist. Intensive Care Med. 2019
- ↑ Sandercock PA and Soane T. Corticosteroids for acute ischaemic stroke. Cochrane Database Syst Rev. 2011 Sep 7;(9):CD000064.