WLAVA: COVID19 ADMINISTRATIVE
Last Updated: 4/19/20
INFECTIOUS DISEASE (ID) ADMINISTRATIVE TOPICS
ID CONTACT INFORMATION
- GLA ID COVID consult p89324 (UCLA).
Misc Numbers:
- Infectious diseases fellow (x40270/40271)
- Microbiology Department (x41259)
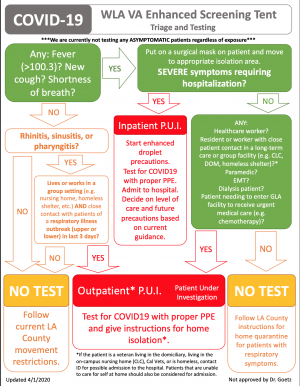
WLA VA ID COVID-19 TESTING ALGORITHM
- Do not need to consult ID to order COVID-19, please review algorithm below to determine if your patient is eligible for COVID-19 testing.
- Reference file (for printing):
CRITERIA FOR ORDERING COVID19 TESTING
- Every admitted patient will receive COVID testing for surveillance.
- For medical admissions we do not wait for the test result before sending patient upstairs.
- Patient does not need isolation precautions apart from when nurses do the swab.
- For psychiatric admission, we DO need to wait for test results.
- If a psych bed is available, order the rapid CEPHEID test with ID/MOD approval to get them upstairs.
- FROM ED:
- Obtain COVID-19 test on all patients admitted to hospital.
- Use PUI criteria to determine level of suspicion for COVID-19.
- Please differentiate between surveillance testing and suspected COVID-19 on EDIS
- Surveillance testing:
- Only reason COVID-19 is being sent is because patient is being admitted to hospital.
- Does not meet PUI criteria.
- DOES NOT NEED ENHANCED DROPLET ISOLATION
- Only reason COVID-19 is being sent is because patient is being admitted to hospital.
- FROM TENT:
- Symptomatic healthcare workers
- Asymptomatic COVID ward attending/resident coming off rotation
- Patient requiring HD
- Patients requiring transfusion/infusion center
- Patients in congregate living or long-term care facility
- Symptomatic healthcare workers
COVID19 TESTS & CHARACTERISTICS
- We have two types of test the Roche (LB send out) and Cepheid test (run in-house).
- The LB test has a turn around time (TAT) ~12-36 hours.
- The Cepheid test TAT ~45min.
CEPHEID COVID-19 TEST
- Very limited availability (only have 20 test kits/week).
- Only order of results will significantly alter the disposition of a patient and/or affects patient flow.
- For example, available inpatient psych beds and a questionably well-appearing symptomatic patient being admitted to psych--- however do not order if we are boarding patients since they will remain in ED anyway and can wait on results
Order process:
- 8a-5p: ID needs to approve (and order).
- 5p-8a: MOD can order it for you.
ED WORKFLOW ADMINISTRATIVE TOPICS
COVID QUICK GUIDE
- File:COVID-19 Quick Guide_042020.pdf
- Last Updated: 4/20/20
- Do not need to consult ID to order COVID-19, please review algorithm below to determine if your patient is eligible for COVID-19 testing.
- Reference file (for printing):
AVOID AEROSOLIZING PROCEDURES (IF POSSIBLE)
- Do not use NEBS - use MDI/SPACER (we have some in stock- if not in FT- check main ED)
- NO to High flow NC (generally - if done place a surgical mask on patient)
- NO to BIPAP
- Intubate early & in a negative pressure room
- AVOID any bagging
MEDICAL STUDENT & RESIDENT RULES REGARDING PUI PATIENT CARE
- Medical students SHOULD NOT participate in any care for COVID — so they don’t spread in their community.
- Residents ok to see PUI patient, but no intubations (includes anesthesia residents).
- Official GLA Housestaff Policy on Residents Caring for COVID-19 Patients:
ED ROOM ALLOCATION FOR PUIS
- Patients with suspected or confirmed COVID-19 disease will be cared for in single rooms with the door closed.
- Airborne isolation rooms (negative pressure rooms) will be used for patients with suspected or confirmed COVID-19 disease who
- Are receiving ICU-level care OR
- Undergoing procedures that are likely to generate a high concentration of respiratory aerosols.
- NOTE: If negative pressure rooms are unavailable for a patient receiving ICU care, patients will be placed in a standard room with staff using N95 with eye protection/PAPRs, gowns and gloves. If hospitalization is not medically needed, home care is preferable if the individual’s situation allows.
LIMITING STAFF EXPOSURE TO PUIS
- We are hoping the following changes in workflow will limit staff exposure to PUIs as well as conserve PPE.
- In stable patients with febrile illness, acute respiratory, or GI symptoms, the nurse will wait until MD assessment to see the patient.
- Please see patient in tandem with resident to limit staff exposure and expedite workups (we can reassess if volumes pick up over coming days).
- This will allow you to practice donning/doffing and creates a buddy system to ensure we are doing it properly.
- Notify nurse of patient's isolation status, place isolation note, and sign isolation order.
- Place all of your workup and treatment orders upfront (including decision on COVID-19 testing) to limit nurse interaction with patient.
- Not all patients need COVID-19 testing, please follow WLA VA ID COVID-19 testing algorithm above. If unsure, consult ID.
CPRS ADMINISTRATIVE TOPICS
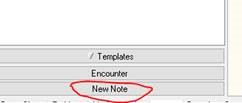
HOW TO PLACE PATIENTS ON ENHANCED DROPLET PRECAUTIONS
- Please have a low threshold to place patients on isolation for COVID-19.
- Start a new note:
- Type in 'Isolation Note:'
- Select Enhanced Droplet Precautions for COVID-19 patients:
- Once you finish the isolation note template, go to 'Orders' menu and sign the isolation order:
iMED CONSENTS FOR COVID19 PUI PATIENTS IN ISOLATION
- Please see pdf (File:Signature Informed Consent for COVID_19_Patients_in_Isolation_Using_iMedConsent.pdf) on how to do this without bringing any equipment or pens into the room
- Basically you sign for them "X"; need 2 witnesses to verify
CRITICAL CARE ADMINISTRATIVE TOPICS
CODE Situation for COVID-19 Cases
- Will be called out as "CODE 99 SPECIAL"
- DO NOT be a hero and RUSH IN
- PPE: N95, Face Shield, bouffant, gloves x2 and gown x2
- Place a surgical mask on patient while getting airway set up, chest compressions ok
- Do not BAG patient
- Limit # of staff
- Staff safety is #1 PRIORITY
MEDICINE INPATIENT ADMINISTRATIVE TOPICS
COVID19 ADMISSION GUIDELINES
- Please have low threshold to admit patients to higher level of care or discuss cases with MOD.
- Draft of COVID-19/PUI Triage Guidelines:
- Most COVID Admissions will go to ICU team
- MICU and SICU teams are sharing the load of PCU/ICU admissions.
- If the patient is stable enough for GMED (see triage guidelines), you can admit to GMED COVID unit
- MICU and SICU teams are sharing the load of PCU/ICU admissions.
- MICU vs SICU Schedule:
- 4/6 through 4/12: Primary team SICU
- 4/13 through 4/19: Primary team MICU
- If 5SD is full, admissions alternate between MICU and SICU
- MOD can help sort any confusion
- New Isolation Note
- Specific to COVID19 - indicate if ICU level of care and high risk for aerosolizing procedures vs usual care.
COVID19 DIRECT ADMISSION GUIDELINES
- Same as our previous direct admission policy.
- Patients in clinic can be admitted directly if stable and clinic is still open.
- Provider that made admission disposition decision must call MOD/OTS for coordination.
- If patient coming from home, provider can still call MOD/OTS. Holding area will be Tent if there is not immediate inpatient bed available.
- Anyone coming from community nursing home that is confirmed COVID+ can be directly admitted as long as they are STABLE.
- Since these patients can deteriorate rapidly, we must make sure they can wait for an available bed without being monitored in the ED.
- This includes ALL community nursing homes, not just the CLC
- OTS or Transfer Office (x31448)
- Call MOD and they will take care of admitting orders
HOMELESSNESS ADMINISTRATIVE TOPICS
DISPOSITION OF HOMELESS PUI PATIENTS
- If homeless and can self-isolate AND does not want to be placed in a shelter
- Discharge with self-isolation instructions
- If homeless and was previously living in a congregate living facility (board and care, shelter) OR requesting housing OR cannot self-isolate AND is able to self care completely
- Social work consult for DOM COVID unit/building 214 (see below for process). The patient does not need to have substance use in order to stay here
- If homeless and patient is not able to self care or has other specific needs
- Admit to medicine 5SD, gmed/PCU/ICU depending on level of clinical care
- If no DOM beds are available
- Consider admitting to medicine
PROCESS OF PLACING PATIENTS IN COVID19 DOM (BLD 214)
- Think of this as a homeless shelter for PUIs with pending COVID test or COVID+. Patients do not need to have substance use issues.
- COVID DOM Checklist (File:COVID-19 B214 ADM-ED.INPT.PACT 04.10.2020.pdf)
- Consult social worker
- Make sure patient ruled out for TB with cxr or quant ifn within the past 12 months. pCXR an be done in the tent if needed.
- Fill out CERS <ATTENDING ATTESTATION-INDEPENDENCE/ELIGIBILITY-CERS PROGRAM>
- Social worker will contact DOM for bed between 8am -10pm. If overnight, will need to be observed
PSYCHIATRY ADMINISTRATIVE TOPICS
PSYCHIATRY ADMISSIONS & SURVEILLANCE TESTING
- Patients cannot go upstairs until COVID negative
- If beds available, order CEPHEID (ID approval 8a-5p, hospitalist overnight)
- If no beds and boarding, order "regular" COVID test (send out to LB).
ED PSYCH OBS
- We are expanding ED psych obs to include all “soft SI admits”. Previously ED psych obs was only for patients that were intoxicated. Given the current environment and to best preserve COVID tests, please allow patients that are conditional SI that are likely to clear by morning time to be placed in ED PSYCH OBS for reassessment by psychiatry in the morning IF there are beds available in the ED.
- If no beds in the ED, please collaborate with the charge nurse to discuss whether it is feasible to keep the patient in a medical bed until the next day. Otherwise, admit to the psychiatric service.
- If the patient is likely to be discharged the next day, DO NOT ORDER A COVID PANEL. There is always the option of ordering a CEPHEID if the patient converts to a true admit.
DETAINING PUI OR COVID19+ CONFIRMED PATIENTS
- It seems that without any specific quarantine order (rare that we will have an official order on our patients)- we cannot detain patients against their will unless we do not think they have capacity- which is a separate issue.
EMPLOYEE HEALTH ADMINISTRATIVE TOPICS
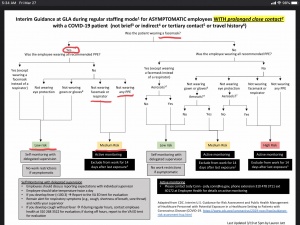
GLA PROVIDER EXPOSURE RISK ALGORITHM
- Please protect yourself from inadvertent exposure by making sure patients that have any hint of being a potential PUI (i.e., epidemiological risk factors, URI sx, any respiratory sx, etc.) are wearing a face mask (can use conical or level 1/yellow mask).
- Reviewing the exposure risk algorithm shows that this simple intervention keeps exposure risk low to medium.
- Second layer of defense is ensuring that you wear a face mask (NOT N95).
- File:20200319.1700.Interim GLA guidance for healthcare monitoring.pdf
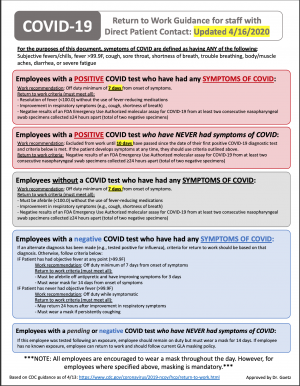
EMPLOYEE RETURN TO WORK GUIDANCE
Last Updated: 4/17/20
YOUR HEALTH (& OURS)
- If you develop a fever and/or resp symptoms- notify Neil/Jonie immediately. We know how hard y'all want to work - but it's important to stay healthy and keep away from others to avoid further spread of disease to coworkers and patients and additional need for quarantine.
OTHER WLA VA PAGES
- WLAVA
- WLAVA:Administrative Handbook
- WLAVA:COVID-19 PPE
- WLAVA:COVID19 ED Airway
- WLAVA:COVID19 ED Operational Updates
- WLAVA:Enhanced Screening Tent
- WLAVA:Enhanced Screening Tent Employee Template
- WLAVA:Enhanced Screening Tent LIP Orientation
- WLAVA:Enhanced Screening Tent Telehealth
- WLAVA:Enhanced Screening Tent Template
- WLAVA: COVID19 ADMINISTRATIVE