Acute angle-closure glaucoma: Difference between revisions
(→Source) |
No edit summary |
||
| (70 intermediate revisions by 20 users not shown) | |||
| Line 1: | Line 1: | ||
== | ==Background== | ||
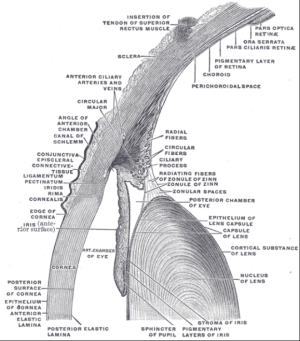
[[ File:Gray883.png|thumb|Eye angle anatomy.]] | |||
[[File:PMC4614311 qmj-2015-01-0006-g002.png|thumb|Mechanism of acute angle closure.]] | |||
* | [[File:PMC3991910 1471-2431-14-96-1.png|thumb|A. Slit lamp exam of the right eye demonstrating diffusely shallow AC, large pupil, and slightly injected conjunctiva. B. Normal slit lamp photograph of the right eye after resolution of acute angle closure C. Anterior segment of the right eye demonstrating abnormal anterior iris convexity, iridocorneal apposition at the angle, and an anterior lens vault D. Normal anterior segment of the right eye demonstrating horizontal iris, no iridocorneal apposition, anterior iris convexity, or anterior lens vault.]] | ||
===Pathophysiology=== | |||
*Obstructed aqueous outflow tract → aqueous humor builds up → increased intraocular pressure (IOP) → optic nerve damage → vision loss | |||
*Increased posterior chamber pressure causes iris to bulge forward (iris bombé) → further obstruction of outflow tract → further increase IOP | |||
*Acute attack is usually precipitated by pupillary dilation | *Acute attack is usually precipitated by pupillary dilation | ||
== Clinical Features == | ==Clinical Features== | ||
[[File:Acute Angle Closure-glaucoma.jpg|thumb|Ciliary/circumcorneal flush and hazy cornea characteristic of acute angle closure glaucoma.]] | |||
[[File:Acute angle closure glaucoma.jpg|thumb|Right eye with mid-sized, fixed pupil and ciliary flush.]] | |||
[[File:PMC4601337 oed-7-2015-021f1.png|thumb|Acute angle-closure glaucoma with mid-dilated pupil and an intraocular pressure of 50 mmHg.]] | |||
*Abrupt onset of severe (usually [[Red Eye (Unilateral)|unilateral) eye pain]] | |||
*[[Blurred vision]] | |||
*Halos around lights | |||
*Frontal or supraorbital [[headache]] | |||
*[[Nausea]] / [[vomiting]] / [[abdominal pain]] | |||
*Fixed, midposition pupil | |||
*Hazy cornea | |||
*Conjunctival injection most prominent at limbus (ciliary flush) | |||
*Rock-hard globe | |||
==Diagnosis== | ==Differential Diagnosis== | ||
{{Unilateral red eye DDX}} | |||
== | ==Evaluation== | ||
#Emergent | [[File:PMC4614311 qmj-2015-01-0006-g001.png|thumb|(A) shallow anterior chamber at presentation (B) closed iridocorneal angles on gonioscopy.]] | ||
# | *[[intraocular pressure|IOP]] >20 mm Hg | ||
*[[Slit lamp exam]] shows shallow anterior chamber and ''cell and flare'' | |||
===Definition: 3 signs + 2 symptoms=== | |||
*At least 3 of these signs: | |||
**IOP >21 mm Hg | |||
**Conjunctival injection | |||
**Corneal epithelial edema | |||
**Mid-dilated nonreactive pupil | |||
**Shallow anterior chamber with occlusion | |||
*At least 2 of these symptoms: | |||
**Ocular pain | |||
**Nausea/vomiting | |||
**History of intermittent blurring of vision with halos | |||
==Management== | |||
''Goal of medical therapy is to 'break the attack' in order to prepare the patient for laser iridotomy.<ref>Primary Angle Closure Preferred Practice Pattern Guideline. American Academy of Ophthalmology. [http://www.aao.org/preferred-practice-pattern/primary-angle-closure-ppp--october-2010 Angle Closure PPP] Accessed 06/17/15.</ref>'' | |||
#Emergent ophthalmology consult | |||
#Recheck IOP at least hourly | |||
#Elevate head of bed to decrease IOP | |||
#Place patient in a well lit room (prevent pupillary dilation) | |||
#Start with a topical beta-blocker, α-agonist and PO [[acetazolamide]] if no contraindications | |||
===Decrease production of aqueous humor=== | |||
'''[[Timolol]] 0.5%''': | |||
*Blocks beta receptors on ciliary epithelium | |||
*1 drop in affected eye, repeat in 1 hour if needed. | |||
'''[[Acetazolamide]]:''' | |||
*Blocks productions of HCO3-, which draws Na+ into the eye; water follows by osmosis to form aqueous humour | |||
*500mg IV or PO (PO preferred unless patient is nauseated) | |||
*Can substitute methazolamide 100mg if patient has renal failure. | |||
*Contraindicated in sickle cell patients | |||
'''Dorzolamide (Trusopt) 2%:''' | |||
*topical carbonic anhydrase inhibitor | |||
*1 drop in affected eye | |||
===α2 agonist=== | |||
'''Brimonidine ophthalmic (alphagan) 0.2%''' OR '''Apraclonidine ophthalmic 1%''': | |||
*α agonist will increase trabecular outflow | |||
*1 drop in affected eye | |||
===Facilitate outflow of aqueous humor=== | |||
'''Pilocarpine 1%–2%:''' | |||
*Parasympathomimetic acts on muscarinic receptors found on iris sphincter muscle → causes muscle to contract → miosis → pulls iris away from trabecular network | |||
*1 drop in affected eye every 15 minutes x 2-4 doses, then every 4 to 6 hours | |||
*Likely does not work until IOP drops below 40-50 mmHg, but still give immediately upon diagnosis | |||
*High-concentration pilocarpine (4%) should NOT be given because it can cause forward displacement of the iris-lens diaphragm. | |||
*'''Note:''' may make fundoscopic evaluation more difficult for ophtho consultant due to miosis | |||
===Reduce volume of aqueous humor=== | |||
These therapies are usually reserved for failure of other treatments. Hyper osmotic agents such as mannitol are effective but are contraindicated in renal failure and can cause hypotension in the volume depleted patient. | |||
*'''[[Mannitol]]''': 1-2 g/kg IV given over 45 minutes to minimize cerebral effecfts (most common) | |||
*'''50% glycerin (Osmoglyn)''' OR '''45% isosorbide (Ismotic)''': 1.5 mL/kg PO (rarely used) | |||
===[[Steroids]]=== | |||
*Topical steroids not indicated during acute attack, but may help inflammation after IOP under control. | |||
**[[Prednisolone]] acetate 1% 1 gtt every 15 to 30 minutes four times, then q1h <ref>Guluma, K., & Lee, J. E. (2018). Ophthalmology. In Rosen's Emergency Medicine: Concepts and Clinical Practice (9th ed.). Philadephia, PA: Elsevier/Saunders.</ref> | |||
==Disposition== | |||
*Admit for definitive therapy with iridotomy | |||
==See Also== | ==See Also== | ||
*[[Eye Algorithm (Main)]] | *[[Eye Algorithm (Main)]] | ||
*[[Tono-Pen use]] | |||
*[[Open-angle glaucoma]] | |||
== | ==References== | ||
<references/> | |||
[[Category: | [[Category:Ophthalmology]] | ||
Latest revision as of 18:04, 4 February 2026
Background

A. Slit lamp exam of the right eye demonstrating diffusely shallow AC, large pupil, and slightly injected conjunctiva. B. Normal slit lamp photograph of the right eye after resolution of acute angle closure C. Anterior segment of the right eye demonstrating abnormal anterior iris convexity, iridocorneal apposition at the angle, and an anterior lens vault D. Normal anterior segment of the right eye demonstrating horizontal iris, no iridocorneal apposition, anterior iris convexity, or anterior lens vault.
Pathophysiology
- Obstructed aqueous outflow tract → aqueous humor builds up → increased intraocular pressure (IOP) → optic nerve damage → vision loss
- Increased posterior chamber pressure causes iris to bulge forward (iris bombé) → further obstruction of outflow tract → further increase IOP
- Acute attack is usually precipitated by pupillary dilation
Clinical Features
- Abrupt onset of severe (usually unilateral) eye pain
- Blurred vision
- Halos around lights
- Frontal or supraorbital headache
- Nausea / vomiting / abdominal pain
- Fixed, midposition pupil
- Hazy cornea
- Conjunctival injection most prominent at limbus (ciliary flush)
- Rock-hard globe
Differential Diagnosis
Unilateral red eye
- Nontraumatic
- Acute angle-closure glaucoma^
- Anterior uveitis
- Conjunctivitis
- Corneal erosion
- Corneal ulcer^
- Endophthalmitis^
- Episcleritis
- Herpes zoster ophthalmicus
- Inflamed pinguecula
- Inflamed pterygium
- Keratoconjunctivitis
- Keratoconus
- Nontraumatic iritis
- Scleritis^
- Subconjunctival hemorrhage
- Orbital trauma
- Caustic keratoconjunctivitis^^
- Corneal abrasion, Corneal laceration
- Conjunctival hemorrhage
- Conjunctival laceration
- Globe rupture^
- Hemorrhagic chemosis
- Lens dislocation
- Ocular foreign body
- Posterior vitreous detachment
- Retinal detachment
- Retrobulbar hemorrhage
- Traumatic hyphema
- Traumatic iritis
- Traumatic mydriasis
- Traumatic optic neuropathy
- Vitreous detachment
- Vitreous hemorrhage
- Ultraviolet keratitis
^Emergent diagnoses
^^Critical diagnoses
Evaluation
- IOP >20 mm Hg
- Slit lamp exam shows shallow anterior chamber and cell and flare
Definition: 3 signs + 2 symptoms
- At least 3 of these signs:
- IOP >21 mm Hg
- Conjunctival injection
- Corneal epithelial edema
- Mid-dilated nonreactive pupil
- Shallow anterior chamber with occlusion
- At least 2 of these symptoms:
- Ocular pain
- Nausea/vomiting
- History of intermittent blurring of vision with halos
Management
Goal of medical therapy is to 'break the attack' in order to prepare the patient for laser iridotomy.[1]
- Emergent ophthalmology consult
- Recheck IOP at least hourly
- Elevate head of bed to decrease IOP
- Place patient in a well lit room (prevent pupillary dilation)
- Start with a topical beta-blocker, α-agonist and PO acetazolamide if no contraindications
Decrease production of aqueous humor
Timolol 0.5%:
- Blocks beta receptors on ciliary epithelium
- 1 drop in affected eye, repeat in 1 hour if needed.
- Blocks productions of HCO3-, which draws Na+ into the eye; water follows by osmosis to form aqueous humour
- 500mg IV or PO (PO preferred unless patient is nauseated)
- Can substitute methazolamide 100mg if patient has renal failure.
- Contraindicated in sickle cell patients
Dorzolamide (Trusopt) 2%:
- topical carbonic anhydrase inhibitor
- 1 drop in affected eye
α2 agonist
Brimonidine ophthalmic (alphagan) 0.2% OR Apraclonidine ophthalmic 1%:
- α agonist will increase trabecular outflow
- 1 drop in affected eye
Facilitate outflow of aqueous humor
Pilocarpine 1%–2%:
- Parasympathomimetic acts on muscarinic receptors found on iris sphincter muscle → causes muscle to contract → miosis → pulls iris away from trabecular network
- 1 drop in affected eye every 15 minutes x 2-4 doses, then every 4 to 6 hours
- Likely does not work until IOP drops below 40-50 mmHg, but still give immediately upon diagnosis
- High-concentration pilocarpine (4%) should NOT be given because it can cause forward displacement of the iris-lens diaphragm.
- Note: may make fundoscopic evaluation more difficult for ophtho consultant due to miosis
Reduce volume of aqueous humor
These therapies are usually reserved for failure of other treatments. Hyper osmotic agents such as mannitol are effective but are contraindicated in renal failure and can cause hypotension in the volume depleted patient.
- Mannitol: 1-2 g/kg IV given over 45 minutes to minimize cerebral effecfts (most common)
- 50% glycerin (Osmoglyn) OR 45% isosorbide (Ismotic): 1.5 mL/kg PO (rarely used)
Steroids
- Topical steroids not indicated during acute attack, but may help inflammation after IOP under control.
- Prednisolone acetate 1% 1 gtt every 15 to 30 minutes four times, then q1h [2]
Disposition
- Admit for definitive therapy with iridotomy
See Also
References
- ↑ Primary Angle Closure Preferred Practice Pattern Guideline. American Academy of Ophthalmology. Angle Closure PPP Accessed 06/17/15.
- ↑ Guluma, K., & Lee, J. E. (2018). Ophthalmology. In Rosen's Emergency Medicine: Concepts and Clinical Practice (9th ed.). Philadephia, PA: Elsevier/Saunders.