COVID-19: Example hospital protocols
All protocols are hospital dependent, please check with your hospital administration for existing protocols
Background
This page is for sharing hospital protocols from various institutions. Please add from your institution.
Example Hospital Protocols on WikEM
- ASPR TRACIE COVID-19 Hospital Triage/Screening Resources [1]
- Brigham & Women's Hospital Protocols- [2]
- Massachusets General Hospital protocols- [3]
- Department of Defense Practice Managment - [4]
- Bedside checklist: File:Harbor COVID checklist v3-21-20.pdf
- Harbor DEM COVID airway management guide File:Harbor COVID Airway Management v3-16-20.pdf
- Proper donning and doffing with reusable goggles and stethoscope File:Procedure for Reuse of Faceshields and Goggles 3-19-2020.pdf
- Summary of Harbor consensus guidelines for COVID ARDS management File:Clinical Cheat sheet.pdf
- SBC Admission Criteria for Patients to NOS Alternative Care Site File:Admission Criteria for Patients to NOS Alternative Care Site V3.pdf
- SBC Treatment Guidelines for Patients at San Bernardino Alternate Care Site File:NOS ACS Patient Care Guidelines V3.pdf
Intubation
- Pre-oxygenation
- NC @ 6 L/min
- HFNC controversial
- Consider facemask or other facial covering to prevent aerosolization
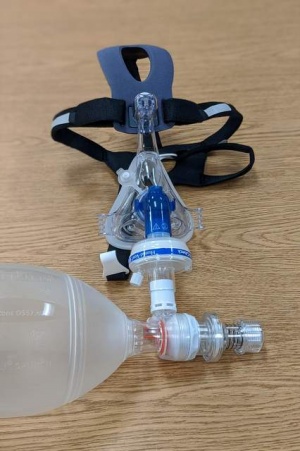
- CPAP mask modified with bio-filter
- If not available, use BVM with bio-filter
- Apneic oxygenation
- Personnel in room
- Intubating physician (most experienced)
- Physician administers meds
- Nurse may enter room once circuit is closed to minimize exposure
- Respiratory therapist
- Intubating physician (most experienced)
- Personnel outside
- Nurse to enter room once circuit closed
- Personnel to record/obtain unanticipated supplies
- Personnel to enter electronic orders if needed
- PPE
- CAPR/PAPR preferred
- Otherwise
- N95 with surgical mask cover recommended
- Eye goggles with side shielding
- Hair cover
- Body suit preferred, otherwise surgical gown
- Double gloves recommended
- Doffing
- All doffing in anteroom preferred
- All PPE except facial covering doffed inside room
- CAPR/PAPR/mask should be doffed immediately outside
- Assign personnel to guide doffing process
- Equipment
- Video laryngoscopy (only bring into room what’s required)
- Direct laryngoscopy NOT recommended
- ETT tube with backup unopened from packet
- CPAP mask or BVM with bio-filter
- Bougie (unopened from packet)
- RSI meds pre-drawn (sedation should be pre-ordered)
- Have other equipment ready for central & arterial lines outside
- Video laryngoscopy (only bring into room what’s required)
- Nursing
- Set up monitor outside door with extension tubings
- Minimize need for mult room entry
- Technique
- Consider using face hood
- RSI by most experienced personnel
- Meds:
- Paralytic: succinylcholine/rocuronium
- Induction: etomidate/ketamine
- Video laryngoscope
- Direct laryngoscopy NOT recommended
- Minimize suction
- Confirm placement with EtCO2 or calorimetric device
- Auscultating for BS not recommended
- Maintain bio-filter inline with ETT at all times
- Ventilation
- Set up pre-intubation
- Lung protective ventilation
- Use ARDSnet
- Vt: 8 ml/kg initially - use predicted body weight
- Target 6 ml/kg
- Goal PaO2 55-80 mm Hg, or SpO2 ≥ 88%
- Plateau pressure ≤ 30 cm H2O
- PEEP: start at 10; be ready to increase
- Use PEEP table to adjust FiO2/PEEP
- Sedation: fentanyl/propofol or ketamine/propofol
- Albuterol: if needed, administer via inline adapter
- HEPA filter as close to patient as possible
- Consider establishing an area for incoming crash intubation from EMS
- It may be more efficient to bring patient to ED room for RSI
- Cover patient's face with mask and/or sheet to minimize aerosolization
- Consider apneic oxygenation during transport to room
- Have pre-designated route to minimize exposure to staff and ED environment
- Receiving team should be transporting patient
- It may be more efficient to bring patient to ED room for RSI
See Also
References
- ↑ https://asprtracie.hhs.gov/technical-resources/119/covid-19-hospital-triage-screening-resources/99
- ↑ COVID-19 Protocols. Brigham and Women’s Hospital COVID-19 Clinical Guidelines. https://covidprotocols.org/protocols/02-ed-inpatient-floor-management-triage-transfers. Published 2020. Accessed April 8, 2020.
- ↑ Massachusetts General Hospital COVID-19 Treatment Guide Version 1.36 04/05/2020. https://www.massgeneral.org/assets/MGH/pdf/news/coronavirus/mass-general-COVID-19-treatment-guidance.pdf. Published 2020. Accessed April 8, 2020.
- ↑ https://www.health.mil/Reference-Center/Technical-Documents/2020/03/24/DoD-COVID-19-Practice-Management-Guide