Reactive arthritis: Difference between revisions
Neil.m.young (talk | contribs) No edit summary |
|||
| (12 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
==Background== | ==Background== | ||
*Historically also known as "Reiter syndrome" | |||
*Seronegative spondyloarthropathy that manifests as an acute, asymmetric, oligoarthritis (LE>UE) that occurs 2-6 weeks after infection | |||
*Patients often positive for HLA-B27 | |||
*Associated with bacterial infections | *Associated with bacterial infections | ||
**Shigella, Salmonella, Campylobacter, Chlamydia, etc. | **[[Shigella]], [[Salmonella]], [[Campylobacter]], [[Chlamydia]], etc. | ||
*Classic triad: [[urethritis]], [[conjunctivitis]], and [[arthritis]] ("Can't pee, can't see, can't climb a tree") | |||
==Clinical Features== | ==Clinical Features== | ||
*Preceding Infection | |||
( | **[[Urethritis]]: generally caused by Chlamydia or Ureaplasma | ||
*Conjunctivitis | **Enteritis: generally caused by Salmonella or Shigella | ||
* | **Respiratory tract infections, both bacterial and viral (case reports have been written about COVID-19 associated reactive arthritis) | ||
* | **Preceding infection may be clinically silent | ||
*Musculoskeletal symptoms | |||
**[[Arthritis]]: oligoarthritis, usually in the lower extremities | |||
**Enthesitis (pain at insertion sites) | |||
**[[Dactylitis]] (sausage digits) | |||
**[[Low back pain]] | |||
*Extra-articular symptoms | |||
**[[Conjunctivitis]] (less frequently [[uveitis]], [[keratitis]]) | |||
**GU symptoms | |||
**Oral lesions | |||
**Cutaneous and nail changes | |||
*Keratoderma blennorrhagicum<ref>Wolff K, Johnson R, Saavedra AP. The Skin in Immune, Autoimmune, and Rheumatic Disorders. In: Wolff K, Johnson R, Saavedra AP. eds. Fitzpatrick's Color Atlas and Synopsis of Clinical Dermatology, 7e. New York, NY: McGraw-Hill; 2013.</ref> | |||
**Develops in 15% of patients | |||
**Found on palm/soles. Vesicles/pustules with yellow/brown color. Appears similar to pustular [[psoriasis]] | |||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
| Line 18: | Line 35: | ||
{{Differencial Diagnosis Migratory Arthritis}} | {{Differencial Diagnosis Migratory Arthritis}} | ||
== | |||
==Evaluation== | |||
*Clinical diagnosis | *Clinical diagnosis | ||
*Must exclude gonococcal arthritis and other | *Must exclude [[Gonococcal arthritis|gonococcal arthritis]] and other mimics | ||
==Management== | ==Management== | ||
* | *Treat inciting infection | ||
* | *Symptomatic treatment of arthritis | ||
* | **[[NSAIDs]] are first line ([[naproxen]], [[diclofenac]], [[indomethacin]]) | ||
**Intraarticular and systemic [[steroids]] for NSAID refractory | |||
==Disposition== | ==Disposition== | ||
| Line 32: | Line 51: | ||
==See Also== | ==See Also== | ||
[[Ankylosing spondylitis]] | *[[Ankylosing spondylitis]] | ||
*[[Gonococcal arthritis]] | |||
[[Gonococcal arthritis]] | |||
==External Links== | ==External Links== | ||
| Line 40: | Line 58: | ||
==References== | ==References== | ||
<references/> | <references/> | ||
[[Category: | [[Category:Rheumatology]] | ||
Latest revision as of 00:31, 13 August 2021
Background
- Historically also known as "Reiter syndrome"
- Seronegative spondyloarthropathy that manifests as an acute, asymmetric, oligoarthritis (LE>UE) that occurs 2-6 weeks after infection
- Patients often positive for HLA-B27
- Associated with bacterial infections
- Shigella, Salmonella, Campylobacter, Chlamydia, etc.
- Classic triad: urethritis, conjunctivitis, and arthritis ("Can't pee, can't see, can't climb a tree")
Clinical Features
- Preceding Infection
- Urethritis: generally caused by Chlamydia or Ureaplasma
- Enteritis: generally caused by Salmonella or Shigella
- Respiratory tract infections, both bacterial and viral (case reports have been written about COVID-19 associated reactive arthritis)
- Preceding infection may be clinically silent
- Musculoskeletal symptoms
- Arthritis: oligoarthritis, usually in the lower extremities
- Enthesitis (pain at insertion sites)
- Dactylitis (sausage digits)
- Low back pain
- Extra-articular symptoms
- Conjunctivitis (less frequently uveitis, keratitis)
- GU symptoms
- Oral lesions
- Cutaneous and nail changes
- Keratoderma blennorrhagicum[1]
- Develops in 15% of patients
- Found on palm/soles. Vesicles/pustules with yellow/brown color. Appears similar to pustular psoriasis
Differential Diagnosis
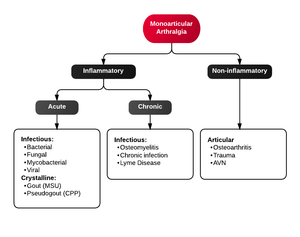
Monoarticular arthritis
- Acute osteoarthritis
- Avascular necrosis
- Crystal-induced (Gout, Pseudogout)
- Gonococcal arthritis, arthritis-dermatitis syndrome
- Nongonococcal septic arthritis
- Lyme disease
- Malignancy (metastases, osteochondroma, osteoid osteoma)
- Reactive poststreptococcal arthritis
- Trauma-induced arthritis
- Fracture
- Ligamentous injury
- Overuse
- Avascular necrosis
- Decompression sickness
- Spontaneous osteonecrosis
- Hemorrhagic (e.g. hemophilia, systemic anticoagulation
- Seronegative spondyloarthropathies (ankylosing spondylitis, IBD, psoriatic arthritis, reactive arthritis
- RA, SLE
- Sarcoidosis, amyloidosis
- Periarticular pathology
- Transient (Toxic) Synovitis (Hip)
- Slipped Capital Femoral Epiphysis (SCFE)
- Legg Calve Perthes Disease
Oligoarthritis
- Ankylosing spondylitis
- Gonococcal arthritis
- Lyme disease
- Psoriatic arthritis
- Reactive arthritis
- Rheumatic fever
- Rheumatoid arthritis
- Systemic lupus erythematosus
Polyarthritis
- Fibromyalgia
- Juvenile idiopathic arthritis
- Lyme disease
- Osteoarthritis
- Psoriatic arthritis
- Reactive poststreptococcal arthritis
- Rheumatoid arthritis
- Rheumatic fever
- Serum sickness
- Systemic lupus erythematosus
- Serum sickness–like reactions
- Viral arthritis
Migratory Arthritis
- Gonococcal arthritis
- Lyme disease
- Rheumatic fever
- Systemic lupus erythematosus
- Viral arthritis
Evaluation
- Clinical diagnosis
- Must exclude gonococcal arthritis and other mimics
Management
- Treat inciting infection
- Symptomatic treatment of arthritis
- NSAIDs are first line (naproxen, diclofenac, indomethacin)
- Intraarticular and systemic steroids for NSAID refractory
Disposition
- Outpatient follow up, with DMARDs if refractory to NSAIDs
- 70% self-limited disease
See Also
External Links
References
- ↑ Wolff K, Johnson R, Saavedra AP. The Skin in Immune, Autoimmune, and Rheumatic Disorders. In: Wolff K, Johnson R, Saavedra AP. eds. Fitzpatrick's Color Atlas and Synopsis of Clinical Dermatology, 7e. New York, NY: McGraw-Hill; 2013.