Sudden sensorineural hearing loss: Difference between revisions
ClaireLewis (talk | contribs) |
|||
| (4 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
==Background== | ==Background== | ||
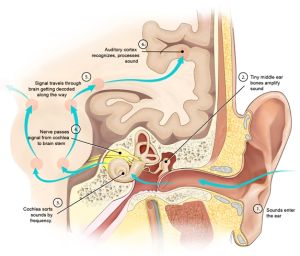
[[File:Hearing mechanics cropped.jpg|thumb|Diagram showing signal processing in the auditory system.]] | |||
===Epidemiology=== | ===Epidemiology=== | ||
*Mostly idiopathic | *Mostly idiopathic | ||
| Line 29: | Line 30: | ||
==Evaluation== | ==Evaluation== | ||
*[[Eponyms_(T-Z)#Weber_test|Weber test]] and [[Eponyms_(Q-S)#Rinne_test|Rinne test]] | *[[Eponyms_(T-Z)#Weber_test|Weber test]] and [[Eponyms_(Q-S)#Rinne_test|Rinne test]] to rule out conductive hearing loss (poor man's version is to have patient hum with mouth closed and ask which side they hear it louder on; ipsilateral for conductive and contralateral for sensorineural) | ||
*Otoscopic exam to rule out OM, OE, foreign bodies, perforated TM or cholesteatoma | *Otoscopic exam to rule out OM, OE, foreign bodies, perforated TM or cholesteatoma | ||
*Remove [[cerumen impaction|impacted cerumen]] and re-examine | *Remove [[cerumen impaction|impacted cerumen]] and re-examine | ||
*Complete [[neurologic exam]] to rule out [[stroke]] | *Complete [[neurologic exam]] to rule out [[stroke]] | ||
*Audiometric evaluation (typically as outpatient) | *Audiometric evaluation (typically as outpatient) | ||
*Consider [[brain MRI|MRI]] to rule out acoustic neuroma, perilymphatic fistula, [[ | *Consider [[brain MRI|MRI]] to rule out [[acoustic neuroma]], perilymphatic fistula, [[Meniere's disease]], vascular insufficiency, [[MS]]; usually can happen as outpatient | ||
*No role for routine laboratory testing or CT head imaging in absence of other findings | |||
==Management== | ==Management== | ||
*Glucocorticoids orally ([[prednisone]] 1mg/kg/day up to 60mg maximum for 10-14 days or [[dexamethasone]] 300mg daily for 3 days) | *Glucocorticoids orally ([[prednisone]] 1mg/kg/day up to 60mg maximum for 10-14 days or [[dexamethasone]] 300mg daily for 3 days) | ||
*Glucocorticoids locally (intratympanic instillation, [[dexamethasone]] 10 to 24mg/mL or [[methylprednisolone]] 30 to 40mg/mL) if refractory to oral GCs | *Glucocorticoids locally (intratympanic instillation, [[dexamethasone]] 10 to 24mg/mL or [[methylprednisolone]] 30 to 40mg/mL) if refractory to oral GCs | ||
*Antivirals for possible [[HSV-1]] infection ([[valacyclovir]] 1g TID or [[famciclovir]] 500mg TID) | *Antivirals for possible [[HSV-1]] infection ([[valacyclovir]] 1g TID or [[famciclovir]] 500mg TID) are not routinely indicated in the absence of exam findings<ref> Clinical practice guideline: sudden hearing loss (update) executive summary Chandrasekhar SS, Tsai Do BS, Schwartz SR, et al. Otolaryngol Head Neck Surg. 2019;161(2):195-210.</ref> | ||
==Disposition== | ==Disposition== | ||
Latest revision as of 22:03, 22 October 2025
Background
Epidemiology
- Mostly idiopathic
- Prognosis depends on severity of hearing loss
- Incidence estimates range from 2-20 per 100,000 people per year
- Most commonly 43-53 years of age
- Men and women affected equally
Clinical Features
- Immediate/rapid hearing loss or hearing loss upon awakening
- Mostly unilateral hearing loss
- Sensation of blocked or full ear, patient doesn’t recognize hearing is gone
- Difficulty in localizing sound
- Tinnitus is common
- Some patients report vertigo
- Occasionally ear pain is present
- No sign of obstruction or otitis media on physical exam
Differential Diagnoses
- Acute stroke, usually AICA occlusion
- Multiple Sclerosis
- Meningitis
- Vestibular schwannomas
- Migrainous infarction
- Acute otitis media
- Traumatic TM rupture
Ear Diagnoses
External
- Auricular hematoma
- Auricular perichondritis
- Cholesteatoma
- Contact dermatitis
- Ear foreign body
- Herpes zoster oticus (Ramsay Hunt syndrome)
- Malignant otitis externa
- Otitis externa
- Otomycosis
- Tympanic membrane rupture
Internal
- Acute otitis media
- Chronic otitis media
- Mastoiditis
Inner/vestibular
Evaluation
- Weber test and Rinne test to rule out conductive hearing loss (poor man's version is to have patient hum with mouth closed and ask which side they hear it louder on; ipsilateral for conductive and contralateral for sensorineural)
- Otoscopic exam to rule out OM, OE, foreign bodies, perforated TM or cholesteatoma
- Remove impacted cerumen and re-examine
- Complete neurologic exam to rule out stroke
- Audiometric evaluation (typically as outpatient)
- Consider MRI to rule out acoustic neuroma, perilymphatic fistula, Meniere's disease, vascular insufficiency, MS; usually can happen as outpatient
- No role for routine laboratory testing or CT head imaging in absence of other findings
Management
- Glucocorticoids orally (prednisone 1mg/kg/day up to 60mg maximum for 10-14 days or dexamethasone 300mg daily for 3 days)
- Glucocorticoids locally (intratympanic instillation, dexamethasone 10 to 24mg/mL or methylprednisolone 30 to 40mg/mL) if refractory to oral GCs
- Antivirals for possible HSV-1 infection (valacyclovir 1g TID or famciclovir 500mg TID) are not routinely indicated in the absence of exam findings[1]
Disposition
Outpatient follow-up with:
- Audiogram in six months after initial diagnosis
- Possible auditory rehabilitation for patients with permanent hearing loss
- Consider assistive hearing devices
Prognosis
- Spontaneous improvement is common
- Better prognosis if high- or low-frequency hearing loss pattern rather than flat across all frequencies
- Around 2/3 of patients will regain hearing in the affected ear
- Worse prognosis in older patients
- Worse in patients with vertigo
See Also
References
- Weber PC. Sudden sensorineural hearing loss. In: UpToDate. Accessed Sept 22 2014.
- Weber PC. Etiology of hearing loss in adults. In: UpToDate. Accessed Sept 22 2014.
- Molina, FJ. Hearing Loss, Chapter 18. Tintinalli’s Emergency Medicine.
- ↑ Clinical practice guideline: sudden hearing loss (update) executive summary Chandrasekhar SS, Tsai Do BS, Schwartz SR, et al. Otolaryngol Head Neck Surg. 2019;161(2):195-210.