COVID-19: Example hospital protocols: Difference between revisions
| Line 32: | Line 32: | ||
*** Consider facemask or other facial covering to prevent aerosolization | *** Consider facemask or other facial covering to prevent aerosolization | ||
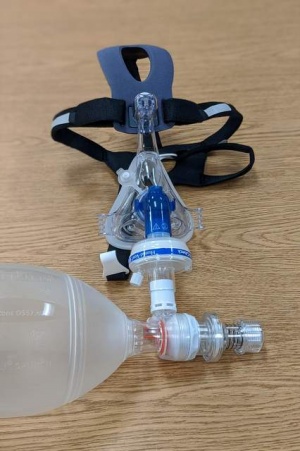
** CPAP mask modified with bio-filter | ** CPAP mask modified with bio-filter | ||
[[File:CPAP with Bio Filter.jpg|thumb]] | [[File:CPAP with Bio Filter.jpg|thumb|CPAP mask with viral filter]] | ||
*** If not available, use [https://www.youtube.com/watch?v=c9h2I8n9Ptk&feature=youtu.be BVM with bio-filter] | *** If not available, use [https://www.youtube.com/watch?v=c9h2I8n9Ptk&feature=youtu.be BVM with bio-filter] | ||
*** Apneic oxygenation | *** Apneic oxygenation | ||
| Line 70: | Line 70: | ||
* Technique | * Technique | ||
** Consider using [https://intubationbox.com/ face hood] | ** Consider using [https://intubationbox.com/ face hood] | ||
[[File:Using Intubation Box.jpg|thumb|Demonstration of an intubation box]] | |||
** RSI by most experienced personnel | ** RSI by most experienced personnel | ||
** Meds: | ** Meds: | ||
| Line 94: | Line 95: | ||
* HEPA filter as close to patient as possible | * HEPA filter as close to patient as possible | ||
* Consider establishing an area for incoming crash intubation from EMS | * Consider establishing an area for incoming crash intubation from EMS | ||
** It may be more efficient to bring patient to ED room for RSI | |||
*** Cover patient's face with mask and/or sheet to minimize aerosolization | |||
*** Consider apneic oxygenation during transport to room | |||
*** Have pre-designated route to minimize exposure to staff and ED environment | |||
*** Receiving team should be transporting patient | |||
==CPR== | ==CPR== | ||
Revision as of 02:43, 13 April 2020
All protocols are hospital dependent, please check with your hospital administration for existing protocols
Background
This page is for sharing hospital protocols from various institutions. Please add from your institution.
Labs/Imaging
- COVID-19 PCR
- Viral panel for alternative diagnosis
- Co-infection with COVID-19 possible
- CBC
- Chem
- LFT
- Sepsis specific labs
- Blood & urine C&S
- Procalcitonin
- Lactate
- Cardiac markers
- D-dimer
- Coagulation panel
- COVID specific panel:
- Ferritin
- LDH
- CRP
- IL-6
- CXR
- POCUS
- CT not recommended for routine evaluation
Intubation
- Pre-oxygenation
- NC @ 6 L/min
- HFNC controversial
- Consider facemask or other facial covering to prevent aerosolization
- CPAP mask modified with bio-filter
- If not available, use BVM with bio-filter
- Apneic oxygenation
- Personnel in room
- Intubating physician (most experienced)
- Physician administers meds
- Nurse may enter room once circuit is closed to minimize exposure
- Respiratory therapist
- Intubating physician (most experienced)
- Personnel outside
- Nurse to enter room once circuit closed
- Personnel to record/obtain unanticipated supplies
- Personnel to enter electronic orders if needed
- PPE
- CAPR/PAPR preferred
- Otherwise
- N95 with surgical mask cover recommended
- Eye goggles with side shielding
- Hair cover
- Body suit preferred, otherwise surgical gown
- Double gloves recommended
- Doffing
- All doffing in anteroom preferred
- All PPE except facial covering doffed inside room
- CAPR/PAPR/mask should be doffed immediately outside
- Assign personnel to guide doffing process
- Equipment
- Video laryngoscopy (only bring into room what’s required)
- Direct laryngoscopy NOT recommended
- ETT tube with backup unopened from packet
- CPAP mask or BVM with bio-filter
- Bougie (unopened from packet)
- RSI meds pre-drawn (sedation should be pre-ordered)
- Have other equipment ready for central & arterial lines outside
- Video laryngoscopy (only bring into room what’s required)
- Nursing
- Set up monitor outside door with extension tubings
- Minimize need for mult room entry
- Technique
- Consider using face hood
- RSI by most experienced personnel
- Meds:
- Paralytic: succinylcholine/rocuronium
- Induction: etomidate/ketamine
- Video laryngoscope
- Direct laryngoscopy NOT recommended
- Minimize suction
- Confirm placement with EtCO2 or calorimetric device
- Auscultating for BS not recommended
- Maintain bio-filter inline with ETT at all times
- Ventilation
- Set up pre-intubation
- Lung protective ventilation
- Use ARDSnet
- Vt: 8 ml/kg initially - use predicted body weight
- Target 6 ml/kg
- Goal PaO2 55-80 mm Hg, or SpO2 ≥ 88%
- Plateau pressure ≤ 30 cm H2O
- PEEP: start at 10; be ready to increase
- Use PEEP table to adjust FiO2/PEEP
- Sedation: fentanyl/propofol or ketamine/propofol
- Albuterol: if needed, administer via inline adapter
- HEPA filter as close to patient as possible
- Consider establishing an area for incoming crash intubation from EMS
- It may be more efficient to bring patient to ED room for RSI
- Cover patient's face with mask and/or sheet to minimize aerosolization
- Consider apneic oxygenation during transport to room
- Have pre-designated route to minimize exposure to staff and ED environment
- Receiving team should be transporting patient
- It may be more efficient to bring patient to ED room for RSI
CPR
- Use auto CPR device if available
- Cover face with plastic or bed sheet to minimize aerosolization
- Minimal personnel
- RT
- 2 providers to switch if manual CPR
- If physician needed for RSI then physician/nurse
- Otherwise nurse/nurse
- Preselected resuscitative meds in bag
- Consider terminating code if no response after pre-planned number of rounds
Asthma
CV procedures
Disposition
- ASPR TRACIE COVID-19 Hospital Triage/Screening Resources [1]
- Brigham & Women's Hospital Protocols- [2]
- Massachusets General Hospital protocols- [3]
- Department of Defense Practice Managment - [4]
- Bedside checklist: File:Harbor COVID checklist v3-21-20.pdf
- Harbor DEM COVID airway management guide File:Harbor COVID Airway Management v3-16-20.pdf
- Proper donning and doffing with reusable goggles and stethoscope File:Procedure for Reuse of Faceshields and Goggles 3-19-2020.pdf
- Summary of Harbor consensus guidelines for COVID ARDS management File:Clinical Cheat sheet.pdf
Example Hospital Protocols on WikEM
See Also
References
- ↑ https://asprtracie.hhs.gov/technical-resources/119/covid-19-hospital-triage-screening-resources/99
- ↑ COVID-19 Protocols. Brigham and Women’s Hospital COVID-19 Clinical Guidelines. https://covidprotocols.org/protocols/02-ed-inpatient-floor-management-triage-transfers. Published 2020. Accessed April 8, 2020.
- ↑ Massachusetts General Hospital COVID-19 Treatment Guide Version 1.36 04/05/2020. https://www.massgeneral.org/assets/MGH/pdf/news/coronavirus/mass-general-COVID-19-treatment-guidance.pdf. Published 2020. Accessed April 8, 2020.
- ↑ https://www.health.mil/Reference-Center/Technical-Documents/2020/03/24/DoD-COVID-19-Practice-Management-Guide