Ketamine: Difference between revisions
| (45 intermediate revisions by 13 users not shown) | |||
| Line 1: | Line 1: | ||
==General== | ==General== | ||
*Type: Dissociative anesthetic | *Type: [[Sedation (main)|Dissociative anesthetic]] | ||
*Dosage Forms: 10, 50, | *Dosage Forms: 10, 50, 100mg/ml | ||
*Routes of administration: IV, IM | *Routes of administration: IV, IM, IN | ||
*Common Trade Names: Ketalar | *Common Trade Names: Ketalar | ||
==Adult Dosing== | ==Adult Dosing== | ||
===Procedural Sedation or Induction=== | ===Procedural Sedation or Induction=== | ||
'''Options: | '''Options:''' | ||
*1 mg/kg IV, followed by 0.5-1 mg/kg IV PRN | *1-2 mg/kg IV, followed by 0.5-1 mg/kg IV PRN | ||
*4-5 mg/kg IM → repeat 2-4 mg/kg IM after 10 min if first dose unsuccessful | *4-5 mg/kg IM → repeat 2-4 mg/kg IM after 10 min if first dose unsuccessful | ||
===Subdissociative Analgesia=== | ===Subdissociative [[Analgesia]]=== | ||
*0.1-0.3 mg/kg IV PRN<ref>Morton NS. Ketamine for procedural sedation and analgesia in pediatric emergency medicine: a UK perspective. Paediatr Anaesth. 2008;18:25-29</ref><ref>Ahern TL, et al. The first 500: initial experience with widespread use of low-dose ketamine for acute pain management in the ED. Am J Emerg Med. 2015 Feb;33(2):197-201. PMID: 25488336. </ref> | *0.1-0.3 mg/kg IV PRN<ref>Morton NS. Ketamine for procedural sedation and analgesia in pediatric emergency medicine: a UK perspective. Paediatr Anaesth. 2008;18:25-29</ref><ref>Ahern TL, et al. The first 500: initial experience with widespread use of low-dose ketamine for acute pain management in the ED. Am J Emerg Med. 2015 Feb;33(2):197-201. PMID: 25488336. </ref> | ||
*Consider giving dose in 100 mL NS bag over 15 min to avoid negative sedation side effects<ref>Motov S, Mai M, Pushkar I, et al. A prospective randomized, double-dummy trial comparing IV push low dose ketamine to short infusion of low dose ketamine for treatment of pain in the ED. Am J Emerg Med. 2017;35(8):1095-1100</ref> | |||
===[[Combative patient]] and/or [[Excited delirium]]=== | |||
*4-6 mg/kg IM or 1 mg/kg IV<ref>Ketamine as Rescue Treatment for Difficulty-to-Sedate Severe Acute Behavioral Disturbance in the ED. Annals of EM. May 2016 67(5):581-587</ref> | |||
===Ketamine Infusion<ref>Miller AC et al. Continuous intravenous infusion of ketamine for maintenance sedation. Minerva Anesth 2011;77:812-20.</ref>=== | |||
*Post-intubation sedation start at 1-2 mg/kg/hr | |||
**Titrate by 0.5 mg/kg/hr q5 min | |||
**Max dose of 4-6 mg/kg/hr | |||
*Field, austere drip<ref>BASIC KETAMINE INFUSION ANAESTHESIA. www.scancrit.com. May 31, 2012. http://www.scancrit.com/2012/05/31/ketamine-infusion-anaesthesia/.</ref> | |||
**Place 500 mg ketamine in 500 cc for 1mg/ml | |||
**Standard maxi drip sets between 10-20 ggt/ml | |||
***Usually 20 gtt | |||
***Mini drip set has 60 ggt/ml | |||
**For quick drip set with 20 ggt/ml | |||
***Use patient's weight in kg (70 kg for example) | |||
***Drip in the same number of drops per min (3.5 mg/min = 210 mg/hr = 3 mg/kg/hr) | |||
==Pediatric Dosing== | ==Pediatric Dosing== | ||
===Procedural Sedation or Induction=== | ===Procedural Sedation or Induction=== | ||
*1.5-2 mg/kg IV '''OR''' | |||
*1.5-2 mg/kg IV | *4-5 mg/kg IM<ref>Green S. et al. What is the optimal dose of intramuscular ketamine for pediatric sedation?. Acad Emerg Med. 1999 Jan;6(1):21-6</ref> '''OR''' | ||
*4-5 mg/kg IM<ref>Green S. et al. What is the optimal dose of intramuscular ketamine for pediatric sedation?. Acad Emerg Med. 1999 Jan;6(1):21-6</ref> | *3-6 mg/kg IN<ref>Hall, D, et al. Intranasal ketamine for procedural sedation. Emerg Med J. 2014; 31:789-90.</ref> '''OR''' | ||
*3-6 mg/kg IN<ref>Hall, D, et al. Intranasal ketamine for procedural sedation. Emerg Med J. 2014; 31:789-90.</ref> | |||
==Special Populations== | ==Special Populations== | ||
*[[Drug Ratings in Pregnancy|Pregnancy Rating]]: B | *[[Drug Ratings in Pregnancy|Pregnancy Rating]]: B | ||
*[[Lactation risk categories|Lactation risk]]: | *[[Lactation risk categories|Lactation risk]]: Infant risk cannot be ruled out | ||
*Renal | *Renal dosing: not defined | ||
*Hepatic dosing: reduce doses, increased duration of action | |||
*Hepatic | |||
==Contraindications== | ==Contraindications== | ||
| Line 43: | Line 55: | ||
*Airway instability (e.g. tracheal stenosis, tracheal surgery) | *Airway instability (e.g. tracheal stenosis, tracheal surgery) | ||
*Active pulmonary infection, including URI or asthma (unless for induction) | *Active pulmonary infection, including URI or asthma (unless for induction) | ||
*CAD, | *CAD, hypertension, CHF | ||
*CNS masses, hydrocephalus (head trauma okay) | *CNS masses, hydrocephalus (head trauma okay) | ||
*Glaucoma/acute globe injury | *Glaucoma/acute globe injury | ||
| Line 49: | Line 61: | ||
==Adverse Reactions== | ==Adverse Reactions== | ||
*Laryngospasm (0.3%) | [[File:Larsons_point.png|thumb|Apply pressure inwardly and anteriorly to the point labeled "Pressure Point" (Larson's Point) while applying a jaw thrust to relieve laryngospasm <ref>Larson CP Jr. Laryngospasm--the best treatment. Anesthesiology. 1998 Nov;89(5):1293-4. doi: 10.1097/00000542-199811000-00056. PMID: 9822036.</ref>]] | ||
** | *[[Laryngospasm]] (0.3%) | ||
** | **Usually associated with large doses or rapid IV push | ||
**Treatment: | |||
**#Jaw thrust | |||
**#Place pressure on Larson's notch | |||
**#If jaw thrust and pressure are not sufficient, bag valve mask with PEEP | |||
**#If above do not resolve laryngospasm, sedate more deeply (propofol is the traditional choice, 0.5mg/kg) | |||
**#If deeper sedation does not resolve laryngospasm, paralyse and intubate | |||
*Apnea or respiratory depression (0.8%) | *Apnea or respiratory depression (0.8%) | ||
**Associated with rapid IV push | **Associated with rapid IV push | ||
**Transient | **Transient | ||
*Hypersalivation (rare) | *Hypersalivation (rare) | ||
**Can pretreat with [[atropine]] or [[glycopyrrolate]]<ref>Green SM et al. Anticholinergics and ketamine sedation in children: A secondary analysis of atropine versus glycopyrrolate. Acad Emerg Med 2010 Feb; 17:157.</ref> | |||
*Emesis, usually well into recovery (8.4%) | *Emesis, usually well into recovery (8.4%) | ||
*Recovery agitation, aka emergence reaction (mild in 6.3%, clinically important in 1.4%) | *Recovery agitation, aka emergence reaction (mild in 6.3%, clinically important in 1.4%) | ||
**Can pretreat with midazolam 0. | **Can pretreat with midazolam 0.05mg/kg (2-4mg for most adults)<ref>Sener S, Eken C, Schultz CH, Serinken M, Ozsarac M. Ketamine with and without midazolam for emergency department sedation in adults: a randomized controlled trial. Ann Emerg Med. 2011 Feb;57(2):109-114.e2</ref> | ||
*Muscular hypertonicity and random, purposeless movements (common) | *Muscular hypertonicity and random, purposeless movements (common) | ||
*Clonus, hiccuping, or short-lived nonallergic rash of face and neck | *Clonus, hiccuping, or short-lived nonallergic rash of face and neck | ||
| Line 72: | Line 91: | ||
*Metabolism: Hepatic | *Metabolism: Hepatic | ||
*Excretion: Urine | *Excretion: Urine | ||
*Mechanism of Action: | *Mechanism of Action: NMDA receptor antagonist | ||
==Comments== | ==Comments== | ||
* | *Give as a slow IV push bolus over 45-60 seconds (rapid bolus increases risk for apnea and laryngospasm) | ||
*IV preferred over IM (faster recovery, less emesis) | *IV preferred over IM (faster recovery, less emesis) | ||
*Nystagmus is seen as an effect of the medication | *Nystagmus is seen as an effect of the medication | ||
* | *Causes sympathetic drive leading to hypertension and tachycardia | ||
**Caution in those with HTN or at risk for CAD<ref>Green SM, Roback MG, Kennedy RM, Krauss B. Clinical practice guideline for emergency department ketamine dissociative sedation: 2011 update. Ann Emerg Med. 2011;57(5):449-461. doi:10.1016/j.annemergmed.2010.11.030 [PubMed 21256625]</ref> | |||
== See Also | ==See Also== | ||
*[[Sedation (Main)]] | *[[Sedation (Main)]] | ||
*[[Procedural Sedation]] | *[[Procedural Sedation]] | ||
*[[Intranasal Sedation]] | *[[Intranasal Sedation]] | ||
*[[Delayed sequence intubation]] | *[[Delayed sequence intubation]] | ||
*[[Ketofol]] | *[[Ketofol]] | ||
| Line 97: | Line 110: | ||
<references/> | <references/> | ||
[[Category: | [[Category:Pharmacology]] [[Category:Critical Care]] | ||
Latest revision as of 21:58, 14 December 2022
General
- Type: Dissociative anesthetic
- Dosage Forms: 10, 50, 100mg/ml
- Routes of administration: IV, IM, IN
- Common Trade Names: Ketalar
Adult Dosing
Procedural Sedation or Induction
Options:
- 1-2 mg/kg IV, followed by 0.5-1 mg/kg IV PRN
- 4-5 mg/kg IM → repeat 2-4 mg/kg IM after 10 min if first dose unsuccessful
Subdissociative Analgesia
- 0.1-0.3 mg/kg IV PRN[1][2]
- Consider giving dose in 100 mL NS bag over 15 min to avoid negative sedation side effects[3]
Combative patient and/or Excited delirium
- 4-6 mg/kg IM or 1 mg/kg IV[4]
Ketamine Infusion[5]
- Post-intubation sedation start at 1-2 mg/kg/hr
- Titrate by 0.5 mg/kg/hr q5 min
- Max dose of 4-6 mg/kg/hr
- Field, austere drip[6]
- Place 500 mg ketamine in 500 cc for 1mg/ml
- Standard maxi drip sets between 10-20 ggt/ml
- Usually 20 gtt
- Mini drip set has 60 ggt/ml
- For quick drip set with 20 ggt/ml
- Use patient's weight in kg (70 kg for example)
- Drip in the same number of drops per min (3.5 mg/min = 210 mg/hr = 3 mg/kg/hr)
Pediatric Dosing
Procedural Sedation or Induction
Special Populations
- Pregnancy Rating: B
- Lactation risk: Infant risk cannot be ruled out
- Renal dosing: not defined
- Hepatic dosing: reduce doses, increased duration of action
Contraindications
- Allergy to class/drug
Absolute
- <3 month old
- Known or suspected schizophrenia, even if currently stable or controlled with medications
Relative
- Major procedures involving posterior pharynx (e.g. endoscopy)
- Typical minor ED oropharyngeal procedures are okay
- Airway instability (e.g. tracheal stenosis, tracheal surgery)
- Active pulmonary infection, including URI or asthma (unless for induction)
- CAD, hypertension, CHF
- CNS masses, hydrocephalus (head trauma okay)
- Glaucoma/acute globe injury
- Thyroid disorder or on thyroid medication
Adverse Reactions
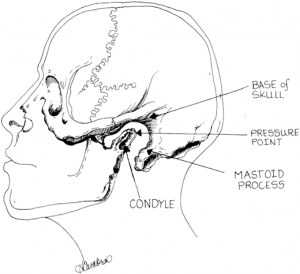
Apply pressure inwardly and anteriorly to the point labeled "Pressure Point" (Larson's Point) while applying a jaw thrust to relieve laryngospasm [9]
- Laryngospasm (0.3%)
- Usually associated with large doses or rapid IV push
- Treatment:
- Jaw thrust
- Place pressure on Larson's notch
- If jaw thrust and pressure are not sufficient, bag valve mask with PEEP
- If above do not resolve laryngospasm, sedate more deeply (propofol is the traditional choice, 0.5mg/kg)
- If deeper sedation does not resolve laryngospasm, paralyse and intubate
- Apnea or respiratory depression (0.8%)
- Associated with rapid IV push
- Transient
- Hypersalivation (rare)
- Can pretreat with atropine or glycopyrrolate[10]
- Emesis, usually well into recovery (8.4%)
- Recovery agitation, aka emergence reaction (mild in 6.3%, clinically important in 1.4%)
- Can pretreat with midazolam 0.05mg/kg (2-4mg for most adults)[11]
- Muscular hypertonicity and random, purposeless movements (common)
- Clonus, hiccuping, or short-lived nonallergic rash of face and neck
Intracranial pressure elevation
- Cerebral perfusion pressure (CPP) was compromised only in the patients with pre-existing intracranial hypertension and obstruction to the flow of cerebral spinal fluid. This has, however, led to the persistent belief that ketamine is contraindicated in patients with traumatic head injuries. Studies done subsequently have shown, however, that the effects of ketamine on cerebral haemodynamics and ICP are in fact variable and depend on both the presence of additional anaesthetic agents and PaCO2 values.[12] Meta-analysis also suggests that Ketamine does not increase ICP and provides favorable hemodynamics.[13]
Neurologic Injury
- Metaanalysis has shown that when ketamine is used in the presence of controlled ventilation, in conjunction with anaesthetics which reduce cerebral metabolism such as GABA receptor agonists, ICP is not increased.[14]
Pharmacology
- Half-life: 2.5 hours
- Metabolism: Hepatic
- Excretion: Urine
- Mechanism of Action: NMDA receptor antagonist
Comments
- Give as a slow IV push bolus over 45-60 seconds (rapid bolus increases risk for apnea and laryngospasm)
- IV preferred over IM (faster recovery, less emesis)
- Nystagmus is seen as an effect of the medication
- Causes sympathetic drive leading to hypertension and tachycardia
- Caution in those with HTN or at risk for CAD[15]
See Also
References
- ↑ Morton NS. Ketamine for procedural sedation and analgesia in pediatric emergency medicine: a UK perspective. Paediatr Anaesth. 2008;18:25-29
- ↑ Ahern TL, et al. The first 500: initial experience with widespread use of low-dose ketamine for acute pain management in the ED. Am J Emerg Med. 2015 Feb;33(2):197-201. PMID: 25488336.
- ↑ Motov S, Mai M, Pushkar I, et al. A prospective randomized, double-dummy trial comparing IV push low dose ketamine to short infusion of low dose ketamine for treatment of pain in the ED. Am J Emerg Med. 2017;35(8):1095-1100
- ↑ Ketamine as Rescue Treatment for Difficulty-to-Sedate Severe Acute Behavioral Disturbance in the ED. Annals of EM. May 2016 67(5):581-587
- ↑ Miller AC et al. Continuous intravenous infusion of ketamine for maintenance sedation. Minerva Anesth 2011;77:812-20.
- ↑ BASIC KETAMINE INFUSION ANAESTHESIA. www.scancrit.com. May 31, 2012. http://www.scancrit.com/2012/05/31/ketamine-infusion-anaesthesia/.
- ↑ Green S. et al. What is the optimal dose of intramuscular ketamine for pediatric sedation?. Acad Emerg Med. 1999 Jan;6(1):21-6
- ↑ Hall, D, et al. Intranasal ketamine for procedural sedation. Emerg Med J. 2014; 31:789-90.
- ↑ Larson CP Jr. Laryngospasm--the best treatment. Anesthesiology. 1998 Nov;89(5):1293-4. doi: 10.1097/00000542-199811000-00056. PMID: 9822036.
- ↑ Green SM et al. Anticholinergics and ketamine sedation in children: A secondary analysis of atropine versus glycopyrrolate. Acad Emerg Med 2010 Feb; 17:157.
- ↑ Sener S, Eken C, Schultz CH, Serinken M, Ozsarac M. Ketamine with and without midazolam for emergency department sedation in adults: a randomized controlled trial. Ann Emerg Med. 2011 Feb;57(2):109-114.e2
- ↑ Filanovsky, Y., Philip Miller et al. Myth: Ketamine should not be used as an induction agent for intubation in patients with head injury. CJEM 2010;12(2):154-7. PDF
- ↑ Wang X et al. Ketamine does not increase intracranial pressure compared with opioids: meta-analysis of randomized controlled trials. J Anesth 2014. PubMed ID: 24859931
- ↑ Himmelseher S. et al. Revising a dogma: ketamine for patients with neurological injury? Anesth Analg. 2005 Aug;101(2):524-34 PDF
- ↑ Green SM, Roback MG, Kennedy RM, Krauss B. Clinical practice guideline for emergency department ketamine dissociative sedation: 2011 update. Ann Emerg Med. 2011;57(5):449-461. doi:10.1016/j.annemergmed.2010.11.030 [PubMed 21256625]


