MVCHC UCC
Location
Mid Valley Comprehensive Health Center (CHC) is located at 7515 Van Nuys Blvd, Van Nuys, CA 91405. It is a 5-floor building containing a variety of primary care and specialty clinics for the Los Angeles County Department of Health Services including Internal Medicine Clinic (2nd Floor), Family Practice Clinic (3rd floor), Women’s Health (3rd floor), Laboratory (3rd floor), UCLA Family Medicine Clinic (4th Floor), and Patient Relations (5th floor). The Urgent Care Clinic (UCC) is located on the 1st floor.
The building is co-located on the same campus as the Zev Yaroslavsky Family Support Center, where there are offices for 7 other LA county agencies including Department of Public Social Services (DPSS) Department of Children and Family Services (DCFS), the Department of Mental Health (DMH), and the Department of Public Health (DPH).
There is ample parking on-site in the adjacent parking structure including several electrical car chargers that are free to use on the side of the garage closest to Mid Valley CHC on the first floor of the structure. There is a strict 4-hour parking rule for the car chargers that is closely enforced.
A map of the campus is below:
MVCHC UCC Mission Statement
We are a dedicated team of health professionals who work to meet the needs of our patients in every circumstance and to provide high value, high quality, efficient care in a safe, patient-centered environment where people love to work and patients choose to come.
MVCHC Guiding Principles
1. Respect. We are a team of equals and we respect one another. We treat our patients with the same respect we treat one another. We appreciate differences in culture, education, abilities, behaviors and lived experience and embrace this diversity as a strength.
2. Quality. We provide the highest quality of care to our patients.
3. Efficiency. We work quickly, creatively, and with urgency to address the needs of our patients as quickly as possible to avoid waits.
4. Value. We challenge ourselves to provide value to the Department of Health Services and its patient population by meeting patient needs, whether acute, chronic or non-medical in nature, and providing assistance in navigating to appropriate services when we cannot meet patient needs.
5. Patient-centered. Excellent service to our patients and effective communication with patients and their families is prioritized in all the care we deliver and services we provide.
6. Growth. Staff are constantly working as a team to grow together to make the Mid Valley Urgent Care a great place to work, where we can all perform at the highest level and constantly grow our skills, relationships and community. 7. Safety. We provide a safe environment for our staff and our patients.
8. Community. We partner with all Mid Valley Comprehensive Health Center staff to be a respected and trusted institution among our community, where community members feel they can go as a safe place for help addressing their needs.
9. Leadership. We consistently innovate to become the Los Angeles County leaders in unscheduled care, providing a blueprint for improvement at other Los Angeles County facilities and supporting others in replicating our success.
10. Support. We help each other when we are in need, and we have each other’s back.
Urgent Care Staff
• The urgent care is staffed with physicians, nurse practitioners, nurses (RNs and LVNs), unit clerks, and patient resource workers (PAC staff) • Unit clerks and PAC staff are assigned to serve the entire urgent care • Providers and nurses are divided into care teams
Care teams
• There are 2 to 4 care teams at any given time in the urgent care built around the provider shifts • A map of the urgent care can be viewed here
• Provider A – assigned to room 3, 4 and 5 • Provider B – assigned to room 1, 2, and 11 • Provider C – assigned to room 8, 9 and 10 • Provider D – assigned to room 6 and 7 • After 8 PM, there are only 2 providers working, and during these times, there will be a combined provider A&B and provider C&D zones • At any given time, RNs and LVNs are assigned to a given care team or to triage/float • Triage/float nurses are expected to triage patients when patients require triage, but otherwise float and help the various care teams as needed • All staff are expected to help other care teams when they fall behind, as needed, with patients, regardless of whether they are assigned to the team
Workflow
Intake
• Patient intake process depends on how sick the patient is (acuity-based workflow) and how busy the urgent care is (capacity-based workflow) • First assess where the patient falls on the acuity-based workflow • Second assess where the patient falls on the capacity-based workflow
Acuity-based workflow
Capacity-based workflow
Registration
• Registration serves 3 purposes o Identify patient and correctly enter to appear on track board o Determine if open PCP appointment and retriage to PCP o Determine if financially eligible to be seen • PAC staff will financially screen patients for eligibility based on information on their PIF or directly talking to patients when there is not a line o Patients financially eligible to be seen should be placed on the trackboard as a “pre-arrival” by PAC staff LVN/RN at registration desk will call patients they see entered as a pre-arrival Before quick registration, LVN/RN should verify patient does not have an existing primary care doctor at Mid Valley with an appointment available – if they do, they should book the patient and send them to clinic After verifying there is no available appointment for the patient, LVN/RN should complete the quick registration from, print a wristband and put it on the patient, and pass the patient back over to registration staff to complete a full registration if they need more information from the patient – in many cases PAC may be able to complete the patient’s registration without talking to them further based on the PIF o Patients deemed financially ineligible (commercial insurance, Medi-cal not assigned to DHS, etc) by PAC, will be called up by PAC prior to placement on the trackboard, and will be offered to pay a flat visit fee of $80 if they would like to be seen. They will also be given information on how to change their insurance to become eligible with patient relations. If they decline the visit fee, they will never go on the trackboard, if they accept the visit, they should be placed as a pre-arrival on the trackboard.
Triage/Intake
• Complete ACN standardized intake questions of UCC, input vital signs • Triage patients by acuity level 1 - Emergent - Sick patient needs to be seen by MD ASAP 2 - Urgent - Patient potentially requiring work up or procedure 3 – Routine - Patient unlikely to require work up or procedure in UCC • When all the rooms are full, and patients are being triaged prior to rooming, patients will be sorted into flows based on their triage-assigned acuity level • Patients will be assigned to providers/roomed in the order that they arrive, but triage level supersedes wait time in terms of priority • For example, if a level 2 patient is in the waiting room and a level 3 patient, the level 2 patient would be assigned/roomed before the level 3, even if the level 3 has been waiting longer
- Fast track will not be a part of the work flow on opening of the urgent care, it eventually may be implemented for level 3’s if there is sufficient volume as hours/staffing expands
Assigning patients to teams
• Patients are assigned by the unit clerk or nursing lead (depending on if a unit clerk is working at that time) to the care team by assigning the patient to the provider on the track board
• As soon as the patient has been registered, they can be assigned to a care team (even while in the waiting room)
• Patients are assigned in a round robin fashion, with a few exceptions:
o Some providers are not trained to see pediatric patients, so these patients cannot/should not be assigned to them, and providers should alert the nursing team at the start of their shift about this
o Patients who are marked as emergent or urgent should be preferentially assigned to physicians over NPs/PAs
• There are limits to the number of patients that can be assigned to a care team in any given hour defined and tracked in this document
• Each black box represents a possible patient that can be assigned in any given hour of a provider’s shift, a new tab will be created for every day and filled as the shift progresses
• The nursing lead assigning patients puts the patient’s initials into the black boxes to indicate a patient assigned in that hour to the care team and then assigns the provider to the patient on the track board
• Care team slots cannot be backfilled. For example, a provider may have 3 slots for 3-4 PM, however, if only 2 patients are assigned by 4 PM, and then 5 patients arrive between 4 and 5 PM that slot cannot be filled
• If there are multiple hours’ worth of patients in the waiting room, patient initials should be written above the slots before the hour actually hits and then moved into the slots when the hour hits. This is to prevent the difficulties issues with sick patients needing to be seen right away when the slots have already been filled for that hour.
• A maximum of 1 patient in queue can be assigned to be seen “early” and placed into the slot for the following hour; this should happen only when a sick patient arrives needing immediate attention and all slots for the hour have already been filled, or when the provider requests to see a patient “early” when they are caught up in the current hour’s worth of patients and want to get started on the next hour.
• Providers can block off an hour for lunch, and they should coordinate with the other providers and nursing working, so that at least 2 providers are always open to patients at any time
• 2 slots may be blocked for patients requiring procedures or patients who are critically ill and are transferred out for admission. For procedures, mark the slot following the slot assigned to the patient “PROC.” For critically ill patients, mark the slot following the slot assigned to the patient “ICU.”
• If it is clear when the patient is assigned based on the triage complaint, a patient will require a procedure or is critically ill, this should be done by the nursing lead/unit clerk when the patient is assigned.
• If it becomes apparent after the provider has evaluate the patient, the provider should alert the nursing lead/unit clerk to block a slot for the procedure or for an “ICU” patient requiring additional time.
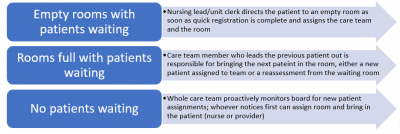
Rooming patients
• Who assigns the patient to the room is based on the scenario, with the goal of getting a patient into a room as quickly as possible in each different scenario
• Patients can be assigned to any room with a few exceptions
o Patients requiring cardiac monitoring, or who are otherwise critically ill should go to bed 2 or bed 3 – an effort should be made to keep patients out of these rooms when they don’t require a higher level of monitoring so that should patients in need arrive, the rooms are available
o Room 9 is a smaller room and is not equipped with a bed, only a chair, so patients requiring a bed for their evaluation or treatment should not be assigned there
Evaluation and treatment of patients
o Rooms 1 and 5 are negative pressure rooms to be used for patients on airborne precautions
• Once roomed, providers should attempt to see and evaluate the patient as soon as possible.
• If a nursing intake has not yet been completed prior to rooming, nursing and providers can/should enter the room together when possible (if not busy with other tasks) to avoid the patients having to repeat their story multiple times.
• After a history and physical, providers can order cardiac monitoring, ECG, labs, x-ray, ultrasound, and PO or IV meds, all to be completed in the urgent care
• If labs/meds are ordered, they should be completed by nursing in the room
• If imaging is ordered or a lab test that takes longer (e.g. urine and the patient can’t go right now or a send out lab we want to await the results of) the patient can be returned to the waiting room to await results after the labs are drawn and meds are given, with the approval of the provider – so that the room can be used to see the next patient
• More information on available labs and medications is below under Laboratory and Medications
Discharge
• Providers should complete discharge instructions and place the “Discharge patient” order
• If the provider is free at the time of discharge, they can print the discharge paperwork and lead the patient out themselves – in which case the provider will bring in their next patient (as under Rooming patients above)
• If the provider is busy at the time of discharge, nursing should print the paperwork as soon as they see the discharge order and lead the patient out – in which case nursing will bring in the next patient (as under Rooming patients above)
Follow up options
As part of an integrated health system, we need to think critically about the necessary follow up plans for every patient discharged from urgent care. We should avoid the common, “Follow up with your primary care doctor in 1-2 days.” Instead there are various levels of follow up options that should be tailored to the need of the patient’s condition, chosen using clinical judgment and clearly communicated to the patient and staff needed to organize follow up. There are 5 general follow-up options for urgent care patients (specialty follow up is more complex and addressed below): 1. Follow up with primary care as needed (this should be most UCC patient visits) a. Patients who are already empaneled to a DHS provider, can make an appointment with their PCP by calling the facility where their PCP is located (this generally name, number, and address generally auto-populates into the follow up section of the patient summary on discharge) b. For patients who are not empaneled (typically relatively new to DHS), you should instruct the patient on how to make an appointment to empanel themselves at their chosen facility. i. Patients can go to http://dhs.lacounty.gov/wps/portal/dhs/locations/ to see a list of all DHS clinics and find the one most convenient to their home. ii. To make an appointment they can call the facility directly and state they would like to establish care with a primary care provider and make their first appointment. iii. Alternatively, patients can call (844) 804-0055 to make an appointment with primary care at any DHS facility. This is sometimes useful because specific facilities may have no new patient appointments available, so patients may get frustrated calling facilities one-by-one. This 844 number can check lots of facilities all at once to find an appointment for the patient. 2. Telephone follow up (TFU) a. A message is sent to the message pool on patient discharge marking the patient as a patient who needs a follow up telephone call the next day to follow up a result or check on a patient’s symptoms 3. Nurse-directed clinic (NDC) a. Patient can be booked into PCMH NDC for symptom recheck or medication titration b. Ask the unit clerk to make an appointment, or if a unit clerk is not working both PAC staff and nursing is able to book appointments c. You need to put detailed instructions for the RN in NDC for what you want them to do, and do not be surprised if nurses running NDC come to ask UCC providers questions about patients sent there for follow up 4. Urgent primary care follow up a. Patient can be booked into an open access or “transitions of care” appointments to follow up with a PCP at Mid Valley b. Even if the patient is not empaneled, they will become empaneled to this provider once they show up for their first visit c. When possible, options 1-3 are preferred when it is safe for the patient, in order to preserve open access/TOC availability as much as possible d. This should only be used when the patient clinically needs to be seen on the scale of days to weeks, rather than month e. Below is a general guide for DHS accepted guidelines for patients that may qualify for urgent primary care follow up following a UCC visit i. New diagnosis or out of control diagnosis requiring close management – cancer, cirrhosis, CHF, DM, CKD nearing ESRD, etc. ii. Recheck of a wound/infection iii. Following up a patient who’s lab were going the wrong direction in the UCC, but doesn’t need admission yet – e.g. worsening anemia, worsening potassium in CKD, etc. iv. Recheck after medication titration of a chronic condition that is losing control – CHF, HTN, DM v. Symptom recheck for patients with cardiopulmonary complaints – e.g. asthma, COPD, CHF, PNA, etc. 5. Return to urgent care for follow up a. Can book the patient into a CCC appointment to return to urgent care itself for follow up b. Can instruct the patient to return without an appointment to urgent care c. Generally, these options are a last resort if all of the 4 options above fail, but for patients who are not empaneled or who you anticipate needing several visits in close succession (e.g. at least 2-3 appointments in <2 weeks) this may be a better option as it is very difficult for primary care in DHS to see a patient multiple times in the space of weeks (rather than months)
Transfer to higher level of care
Patients that cannot be served in the MVCHC UCC fall into 4 categories of action below. Staff should be enlisted to help the provider make these phone calls and coordinate care (may be unit clerk, charge nurse, or other available nursing staff).
1) Call 911 for immediate emergent transfer out
a. STEMI, acute stroke (<24 hours of sx), laboring mother with imminent delivery of infant, persistently hypotensive or hypoxic patients, intractable seizures, airway compromise, patients meeting EMS trauma activation criteria, and other immediately life threatening conditions
b. EMS responds in 5-10 minutes – have as much information for them available and ready to when they arrive as possible, print facesheets, any ECG or labs results, and be ready to give report
2) Call “non-emergent transportation” (NEMT)
a. Who to call depends on the patient insurance status
i. Call the Car (for LA Care patients requiring transportation) – 877-431-2273 / 888-839-9909 / 626-298-8172
ii. Logisticare (for HealthNet patients requiring transportation) – 866 – 842-0675
iii. Medical Alert Center/County Dispatch Office (for all other insurance) - 866-940-4401; press "1" for emergent, or press "3" for DHS facility
b. Patients likely to require hospital admission where there is a significant threat of rapid decompensation in the near future (e.g. upper GI bleed, stable cardiac arrhythmias (e.g. afib with RVR and normal BP), anaphylactic reactions, etc.)
c. Patients likely to require hospital admission who are unable to transport themselves in a safe manner to an emergency department (e.g. they don’t have a car or other means of transportation and do not appear that they could reliably navigate public transportation).
3) Discharge the patient and advise them to go to an emergency department (or the Olive View UCC).
a. Patients where an appropriate work up or treatment requires testing not available in the Mid Valley Urgent Care, but you feel they can be safely transported by private vehicle to an emergency department (e.g. a patient who is otherwise stable but requires CT or MRI imaging or a patient in need of a procedure that requires procedural sedation).
b. If the additional testing required doesn’t need to be done in <24 hours, please consider ordering it as an outpatient and having the patient return to follow up results, rather than sending the patient to an emergency department.
c. For some stable patients, it may be appropriate to send them to the Olive View Urgent Care Clinic, where they have access to the full radiology and laboratory services of Olive View Medical Center in order to avoid an unnecessary ED visit – the OVMC UCC hours are 8AM-10PM Monday – Friday, and 8 AM – 4PM on Saturdays
4) Call the sheriff at X 73190 to place the patient on a 5150 hold and transfer to an LPS receiving facility (the Lanterman–Petris–Short (LPS) Act delineates how involuntary holds are handled in the state of California)
a. Patients who are a significant danger to themselves, others, or gravely disabled who would require a 1-to-1 sitter in an inpatient setting
Follow Up Care
Primary Care
• By default, patients should be provided the phone number for Mid Valley, (818) 627-3000, to establish care/make an appointment at Mid Valley as well as the general primary care scheduling line, (844) 804-0055, if they would like to establish care elsewhere in the county
• It should be noted that patients can only be scheduled into new patient appointment slots from the general primary care scheduling line, however, if a patient calls a specific facility directly, there are sometimes other appointments types that can be booked, even if a patient is told there are no appointments available at that facility
• For patients who have a clear need for ongoing primary care, do not have a primary care doctor, and who are open to getting their care at Mid Valley, an appointment can be booked directly from the urgent care clinic by the unit clerk, nursing, or PAC staff
• Of note, the patient will not be officially “empaneled” until they go to their first primary care appointment
• If a patient is likely to require numerous appointments in a short period of time (e.g. new diagnosis of diabetes, cancer, etc.), managing the patient in the CCC clinic (more information in the CCC section of this document) for a short period of time may be a better option than sending the patient to primary care right away, as typical return appointments in DHS primary care are usually months apart
Specialty Care
• Los Angeles County DHS has a full spectrum of specialty care services available
• (Nearly) all of these services can be accessed through the econsult system
• Econsult is a system that allows referral to specialty care on a non-emergent basis (referrals generally take 1-2 months or more)
• If you feel a patient requires specialty care, you can access econsult from the patient chart by clicking the econsult link in the lower left-hand corner of the patient chart, selecting the appropriate service and filling out the econsult
• Please note that all econsults to dermatology require that a photo of the patient condition be attached, this is generally easiest to accomplish from the “724” down time computer on the large island adjacent to registration, as files can be saved to that computer locally (and cannot be on other devices)
• Please be aware that DHS relies heavily on specialists giving advice through econsult to help non-specialists manage conditions, as their limited in-person appointments are heavily oversubscribed, so the result of an econsult will not always be a face-to-face appointment, but may be a suggestion or additional work up or treatment. A few services are actually “advice only” and will never result in a face-to-face appointment.
• Please read the instructions carefully when completing an econsult, as many common conditions have the expected management practices listed on the econsult page for a given specialty. If you send econsult referrals without following the instructions on the pages, the econsults will be rejectecd. Some specific conditions (e.g. hernia, gall stones) require you to fill out a specific form along with the econsult in the econsult system
• On a daily basis econsults sent from the MVCHC UCC will be reassigned to full-time staff, so if part-timers send econsults, full-time staff can follow up on the recommendations/results of the consult request
• For referrals to specialty care that need to be seen in 1-2 weeks, there are a series of message pools for urgent referrals to Olive View specialty clinics that should be used very sparingly, all of their names begin with “OVM”
• For people who need to see a specialist emergently (within 24-48 hours) they can be sent to the Olive View Medical Center Urgent Care Clinic (UCC) or the LAC+USC UCC where all the on-call specialist services available to those services are available to see patients in the UCC as well
• In general, OVMC UCC is more convenient for patients, however, neurosurgery is not available at OVMC and orthopedic surgery at OVMC cannot operate on joints (e.g. broken hip), so if patients have either of those needs, they should go to LAC+USC
• OVMC UCC hours are 8 AM – 10 PM Monday – Friday and 8 AM – 4 PM on Saturdays; LAC+USC UCC hours are 8 AM – 7 PM Monday – Saturday
MVCHC Bookable Resources
• While most specialties that have clinics at MVCHC require you to get an appointment via econsult, there are a variety of appointment types that can be booked directly from the UCC
• Medical-Legal Partnership (MLP)
o Appointment with a lawer. Lawyers run a clinic at Mid Valley on the 5th floor Mondays and Tuesdays 8-4:30pm. Contact patient relations to make an appointment for your patient with the lawyers to address any kind of legal issue, including concerns around immigration status, eligibility for certain benefits, disputes with landlords, or family law issues.
• Patient education
o 1-on-1 appointments are available with health educators who need education on specific chronic disease/health needs
o Group classes – every month there is a whole calendar of classes available to patients, ask nursing for this month’s calendar, these generally include classes on losing weight, managing chronic disease, smoking cessation – here is an example calendar
• Procedure clinic (Mid Valley Family Medicine)
o Generally, the UCC itself should do procedures when possible, as the appointment slots are limited and are scheduled months out, however, if for some reason it cannot be done in UCC, booking follow up in this clinic is an option
o A clinic that does a variety of procedures including:
Steroid injections (greater troch bursitis, knee, shoulder, trigger finger, lat epicondyle, de quervain's) ** please have xrays for knees and shoulder
Ingrown toenail/partial toenail removal
Trigger point injections
I&D
Skin biopsies (punch/shave)
Wart treatment
Bartholin gland abscess/cyst I&D
Small foreign body removal
Laceration – sutures/suture removal
Liquid nitro to AKs
o Procedures that CANNOT be done in this clinic include:
lipoma removal
Cyst removal (superficial epidermal cysts)
Skin tags
• Musculoskeletal clinic (sports medicine)
o Generally so oversubscribed patients should not be sent from UCC to this clinic, however can be booked if patient is already followed by this clinic
o Abilities of this clinic include:
o Corticosteroid injections:
shoulder (subacromial bursa, AC joint)
elbow (lateral and medial epicondyle)
hand (1st CMC arthritis, De Quervain, trigger finger, Carpal Tunnel)
hip (trochanteric bursa, NOT hip joint
knee (joint, anserine bursa, IT band bursa at lateral femoral condyle)
ankle (joint, sinus tarsi, Morton Neuroma, 1st MTPJ arthritis/Gout)
o Aspiration:
Ganglion cyst (wrist, hand, ankle)
symptomatic knee effusion
Laboratory
• At the time of the opening of MVCHC UCC point-of-care testing was in flux due to issues surrounding pending laboratory license, please check in with staff whether a certain test is available in the MVCHC UCC before ordering it until the full menu of testing becomes standard
• Point-of-care testing is available on site, we have the following tests available:
o Abbott i-Stat
Chem8+ cartridge - Chem 7 + Hgb/Hct
EC8+ cartridge – Na, K, Chloride, Anion Gap, Glose, BUN, Hgb/Hct, pH, pCO2
Cr cartridge – separate from EC8+
Beta-hCG – serum quantitative
Troponin
PT/INR
Planned to stock, but currently has manufacturer issues CG4+ cartridge (Blood gas and lactate)
o Clinitek
Urine hCG
Urinalysis
o Glucometer
Glucose
o Hemoccue
Hemoglobin
• Any other laboratory testing in the DHS system can be ordered, but is delivered via courier to the Olive View laboratory for process
• Courier pick ups currently occur at 12PM and 8 PM, but are planned to expand to every 4 hours at 12 PM, 4 PM, 8 PM, and 12 AM
• Turnaround time on even simple send out labs can be as much as 5-6 hours depending on the timing it is ordered
• The Olive View lab can be contacted for questions at (747) 217-4977
• Patients should generally not be held in the urgent care awaiting lab results of labs that are not point-of-care labs performed in the urgent care
• Providers can send a message to the telephone follow-up pool to follow up labs ordered in the urgent care, which they do not feel they can follow up themselves in a timely fashion themselves and for which the results may require timely action
• If a provider feels a patient should not be sent home without the results of a certain laboratory test, they should strongly consider sending the patient to an emergency department to have the test done, rather than holding the patient in the urgent care for the test results
• Generally testing of difficult to obtain bodily fluids should not be sent from the urgent care, such as cerebrospinal fluid (CSF), ascites fluid, pleural fluid, synovial fluid, etc. as there is a risk of the samples being lost or improperly processed in transit to Olive View, if a diagnostic test is urgently required on these fluids the patient should be sent to the Emergency Department
Imaging
Radiology
• Olive View Radiology Department reads plain films and ultrasounds for Mid Valley
• General radiology is staffed 7AM – 5PM Monday - Friday and 7AM – 1 PM on weekends, they will read any stat plain films as well as ultrasounds with a ~1 hour turnaround time
• ED radiology is staffed until 11 PM Monday - Friday and until 7 PM on weekends. ED radiology will read ultrasounds, but they do not routinely put in formal reads on plain films.
• If you get a plain film after general radiology hours and you want help with a read (or other times you want help with a read), you can call the ED radiology reading room at Olive View at (747) 627-4969 or (747) 627-4971
• If you get imaging when the ED radiology room is not staffed, it will not be read until the next day
X-ray
• X-ray is available on site for all hours the urgent care is open
• When an x-ray is ordered, the x-ray tech should look at the track board to determine the location of the patient (a room vs. waiting room), get the patient, and bring them to perform an x-ray in the x-ray suite
• If all that remains for a patient’s work up is an x-ray, urgent care staff can also bring the patient directly to the x-ray tech to expedite the patient’s disposition
• A portable x-ray machine is also available to the urgent care, but ordering of portable x-rays should be reserved for patients who cannot be transported to the x-ray suite and providers should only order portable films to be taken in rooms where the machine can actually fit (e.g. it may work well in the observation beds, but a portable x-ray machine cannot fit in room 9)
• When ordering portable x-rays, please contact x-ray tech to let them know
Ultrasound
• Ultrasound is available on site during Mid Valley clinic hours (8AM-8PM Monday – Thursday and 8 AM to 5 PM on Friday)
• When an ultrasound is ordered, nursing/the provider should contact the ultrasound tech, who will give you an approximate time they would like to see the patient to complete the scan and that patient should be brought over at that time
CT/MRI
• CT and MRI are NOT available on site
• If a patient requires a CT or MRI, they can be ordered as a future order in Orchid to be scheduled at Olive View – please keep in mind that if you do not plan on following up the result of this imaging test yourself, you should send a message to the telephone follow up pool to ensure that it is followed
• If the CT/MRI is not urgent, it will be scheduled 1-2 months
• If you have an urgent CT that needs to happen in <2 weeks, in addition to placing a future order, you should ALSO send a message to “ACN – MVC UCC to Radiology CT Urgent” message pool through the internal messaging feature in Orchid from the patient’s chart explaining why the CT is required within 2 weeks
• If a patient needs a CT or MRI the same day, they need to be sent to the Olive View emergency department; Olive View does not have MRI available in the ED after midnight on weekdays or on the weekends, so the patient needs an MRI and would be arriving in the ED at Olive View during one of these times, they should be preferentially sent to Harbor or LAC+USC ED
• If a patient is stable, but needs same day imaging per clinical judgment, this is not an indication (necessarily) for ambulance transport – if they are stable, they can be instructed to self-transport to an ED for imaging
Mammogram
• Mammograms are done at Mid Valley, but they cannot be done in the urgent care, they can be ordered on urgent care patients as a future order to be done at Mid Valley Radiology.
Medications
A full list of the available medications available for order to be given in the MVCHC UCC is here. There is also a binder with a list of the meds stored in the pyxis on the pyxis machine.
Storage
• Medication, both PO and IV medications are available and accessible through the Pyxis ES Device. Pyxis ES Device is linked to the Tower and the refrigerator. The Tower contains large volume IVs, Pre-mixed IV Antibiotics, as well as bulk oral and/or topical medication. The refrigerator contains mostly vaccines in addition to medications (non-vaccines requiring refrigeration). Pyxis Main Frame, contains oral, IV, and topical medications.
• Crash Cart medication tray is available. Back up medication supply that is in the crash cart medication list is also available in the Pyxis.
Medication Access
• Pyxis ES access is available through request to the pharmacy department (818-904-5505) which is granted based on approved roles. (Form for user access is available in Pyxis folder located on top of small refrigerator next to Pyxis ES)
o Pyxis ES Access is through ADT. It requires employee number and Windows/E-mail password to initiate set up. BioID set up is required.
In case the Bio-ID is not recognized and account is locked, password reset will be required by going to a desktop and access homepage to reset password. The reset password needs to be communicated to the pharmacy department to sync the reset password to Pyxis (otherwise, you will need to wait for programmed sync which is every 4 hours).
Notes from Pharmacy Team
• Medication is stocked for clinic use to be administer by the medical team. Medication should not be given to the patient to take home and consume at home. This will violate number of Ca Board of Pharmacy labeling and counseling requirements.
• If a medication is not available in the Pyxis machine for 1st dose administration and it does not need to be administered emergently, the medication should be e-prescribed as an outpatient prescription and filled at our pharmacy next door or any commercial pharmacy.
Pharmacy
• DHS Formulary is available online as a tool to reference if prescribed medication is in DHS formulary and formulary restrictions (include Prior Authorization Forms). Go to the home page and click the link called “DHS Core Formulary.”
• DHS Formulary restrictions should be observed and when possible, formulary medications should be selected for the patient. If a medication is non-formulary, a non-formulary form should be fill out to facilitate timely prescription processing by the pharmacy department to better serve patients.
• All medications should be eprescribed, including controlled substances.
• CURES database must be reviewed for each patient prior to e-prescribing any narcotic substance.
• Controlled substances are prescribed using the Imprivata app, you can call the Enterprise Help Desk for help getting enrolled in this, but will eventually have to talk to our local IT person, Scott Cain at extension x73080, to get your phone set up as a verification device
• There is a DHS pharmacy on site in the bottom floor of the Zev Yaroslavsky Family Support Center with an entrance on Van Nuys Blvd right next to the Mid Valley Comprehensive Health Center. In Orchid it is labeled “LA CO ACN Mid-Valley CHC (7555 Van Nuys Blvd)”.
• The pharmacy hours match the urgent care opening hours, any prescriptions for a patient should be written at least 30 minutes before closing to ensure that the pharmacy can fill it before they close
• You can call the Mid-Valley pharmacy at (818) 904-5505 with any questions.
• A list of some commonly topical agents that are kept in stock in the pharmacy which can be easily/quickly filled when prescribed as an outpatient is available here
Procedures
Providers who feel comfortable with the following procedures should feel welcome to perform these procedures in the urgent care:
• Laceration repairs*
• Suture and staple removal*
• Trephination of subungual hematoma*
• Hernia reduction (not requiring procedural sedation)*
• Abscess incision and drainage*
• Closed fracture reduction and splinting* (not requiring procedural sedation)
• Removal of foreign body superficial embedded in skin (e.g. splinters)*
• Closed joint dislocation reduction (not requiring procedural sedation)
• Bartholin’s gland cyst incision and drainage
• Felon/paronychia drainage
• Joint aspirations and injections (therapeutic)
• Epistaxis control measures (e.g. nasal packing)
• Removal of foreign body from ear, nose, vagina, rectum (if superficial), or eye (around exterior globe/cornea)
• Ring removal
• Low risk nerve blocks (e.g. digital block, dental block, etc)
• Bladder catheterization
• Compartment pressure measurement
• G tube replacement
• Superficial hemorrhage control (e.g. bleeding varicose vein)
• Needling and trigger point injections
• Manual manipulation for musculoskeletal pain
• Application of sealant to fractured tooth with exposed dentin – or splint for dental trauma
• External jugular IV placement
• Ingrown toe nail removal
• IUD removal
Providers who do not feel comfortable with any of these procedures, but encounter a patient in need, should ask the other provider on if they are comfortable prior to sending the patient out and, if interested, take the opportunity to learn these procedures.
At a bare minimum, all providers should be able to perform the procedures with an asterisk (*). If, at the time of onboarding a provider is not comfortable with these procedures, they will be provided opportunities to train in order to achieve a comfort level necessary to perform them.
Before all procedures, it is required that a patient (or representative) sign an iMed consent form for the procedure and that a time out is taken.
This list is not meant to be exhaustive. Providers should use their best judgment. Any procedures attempted in the Mid Valley Urgent Care should prioritize patient safety above all else. Procedural sedation, or procedures requiring procedural sedation, should not be attempted in the UCC given the lack of a ventilator available. If the provider is concerned it is an unsafe setting to perform a given procedure, they should send them to an emergency department or other setting where the procedure would be safe to perform.
Condition-specific protocols
Chest pain
• Register patient and select “cardiac” during quick registration to autogenerate an ECG order
• Inform triage nurse for chest pain protocol
• ECG done within 10 minutes and shown to physician
o STEMI or STEMI equivalent (e.g. wellen’s) – Call 911 for transport to nearest ED
o Ischemic ST depressions with active chest pain - Call 911 for transport to nearest ED
o All other ECG findings – provider should use clinical judgment to evaluate patient risk further before calling 911 and consider alternative options under “Transfer for higher level of care” above
• If calling 911 – anticipate arrival in 5-10 minutes at most
o Room in observation bed awaiting EMS arrival on cardiac monitor
o Defibrillator/crash cart at bedside
o Place 1 IV (2 if time)
o Give aspirin, nitroglycerin, and oxygen
o Print patient facesheet and ECG copies to provide to EMS
o Physician report to EMS on arrival
o If patient refuses 911 transport, sign out AMA
• If evaluating patient further
o Place 1 IV (2 if time)
o Room in observation bed on cardiac monitor
o Labs, imaging, and medications per physician order
o If low risk by HEART score, consider discharge with negative troponin
o If higher risk, consider the options under “Transfer for higher level of care” above
Possible Stroke
• If patient informs staff in registration “I think I’m having a stroke” or has characteristics of a stroke patient, notify triage nurse
• Triage RN & physician
o Assess for signs and symptoms: Slurred speech, facial droop, confusion, and extremity numbness/weakness.
o ASSESS FOR LAST KNOWN WELL TIME
o Check glucose
• If <24 hours of neurological symptoms that provider feels are consistent with a stroke, call 911 for transport to the nearest stroke center emergently
o Room in observation bed awaiting EMS arrival on cardiac monitor
o Defibrillator/crash cart at bedside
o Place 1 IV (2 if time)
o Print patient facesheet to provide to EMS
o Physician report to EMS on arrival
o If patient refuses 911 transport, sign out AMA
• If >24 hours of symptoms, physician can evaluate further in the urgent care.
Consider transferring patient out if there is need for CNS imaging through any of the options listed under the “Transfer to higher level of care” section
Pregnancy
• Patients less than 14 weeks EGA with any type of complaint will be triaged and seen as a regular patient by provider
• Patients who are 14 WEEKS EGA AND ABOVE who complain of the following symptoms: abdominal pain, vaginal bleeding, pelvic pain, flank pain, headache, or high blood pressure
o Provider to screen up front to determine no need to call 911; as long as patient does not need 911, should be redirected to OBYGN: OVMC L&D 3rd floor or follow up with patient’s own private provider
o If complaint appears to be completely unrelated to pregnancy, e.g. a sprained ankle, OK to evaluate that complaint in urgent care first and check patient in and then send to OBGYN for follow up after urgent care visit
• If sending to Olive View L&D
o Notify at (747) 210-4462 with
NAME OF PATIENT
MRN
D.O.B.
EGA
COMPLAINT
• TERM PREGNANCY PATIENTS WHO WALK IN AND COMPLAINS OF RUPTURE OF MEMBRANE OR OTHER SIGNS OF ACTIVE LABOR
o Room in observation bed awaiting EMS arrival on cardiac monitor
o Place 1 IV (2 if time)
o Print patient facesheet to provide to EMS
o Physician report to EMS on arrival
o If patient refuses 911 transport, sign out AMA
• POST PARTUM PATIENT WITH NEONATE - Call 911
o Room in observation bed awaiting EMS arrival on cardiac monitor
• Assess patient and neonate
• If post-partum patient with unresponsive neonate – Call 911
o CODE BLUE
Psychiatric complaints
• If a walk-in patient complains of SI/HI during registration:
o Inform TRIAGE NURSE
Assess patient
NOTIFY PROVIDER
• ROOM PATIENT 1:1
o PROVIDER will assess the need for a psych evaluation.
• If medically cleared by provider, patient is discharged and referred to Mental Health Urgent Care (discharge patient with resources).
• If patient potentially qualifies for a 5150 hold on evaluation per provider: CALL SHERIFF X 73190
• If patient is placed on a 5150 hold, provider medically clears patient.
Patient transferred to nearest PSYCH facility via Sheriff or FIRE dept.
• If patient is NOT placed on a 5150 hold by Sheriff:
Document police officer’s name, badge number, and department
o Notify provider and discharge patient with proper resources
F.Y.I. 24 HOUR SUICIDE PREVENTION CENTER HOTLINE (877) 727-4747
• If patient is not placed on a 5150 hold AND the provider deems the patient mentally unstable for discharge, collaborate with Sheriff in order to provide appropriate care.
o Document police officer’s name, badge number, and department
• Psychiatric Emergency Teams (PET) are mobile teams operated by psychiatric hospitals approved by the Department of Mental Health to provide 5150 and 5585 evaluations. Team members are licensed mental health clinicians. PET operates similar to PMRT and provides additional resources in specific geographical regions. For contact information on PET, call (800) 854-7771. PET Teams take a long time, so Sheriff involvement, who is much quicker to respond should be prioritized over PET.
• IF THE PATIENT LEAVES THE URGENT CARE REGARDLESS IF PATIENT IS ON A 5150 HOLD, DO NOT FOLLOW PATIENT. CALL SHERIFF X 73190 / 911.
Victims of Abuse
• ANY PATIENT THAT WALKS IN REPORTING OF ABUSE
• Notify triage nurse & provider
• ROOM PATIENT for further assessment by triage nurse/provider. Document OBJECTIVELY. Interview patient privately.
• (If patient needs to void, collect urine for possible evidence and label specimen)
• FOR PEDIATRIC PATIENTS:
o Interview patient and family separately if possible (possible abuse from a family member)
o If patient needs to be placed in a gown for further assessment, place clothing in a plastic bag with patient label
• Call Sheriff X73190 to evaluate the need for law enforcement report.
o SHERIFF communicates other police department (depending on where event took place)
• Resources
o Center for Assault Treatment Services (C.A.T.S.) –Northridge
o Adult protective Services (213) 351-5401
o Suspected Child Abuse Hotline (800) 540-4000
o http://lacdcfs.org/
o Social workers on call at OVMC
• DISCHARGE PATIENT PER PROVIDER WITH RESOURCES
• Please recall that health care providers are mandated reporters in California for certain populations, you can follow guidelines here
Sepsis
• TRIAGE NURSE: Any patient that MEETS 2 of the following: o Temperature > 100.4 (38 C) or <96.8 (36 C) o HR > 100 BPM o RR > 20 o SBP < 90 o AND Patient has a suspected infectious source • ROOM PATIENT AND NOTIFY PROVIDER o Per provider, expedited work up Lab draw – blood culture, CG4+, CHEM8+ UA CXR IV placement – antibiotics and fluids ASAP • Consider “Transfer to a higher level of care” per the protocol above
Substance Use Disorder
• DHS prides itself on a harm reduction approach to substance use disorder (SUD) • Our goal is to meet patients where they are at and provide them any resources we can to make their SUD safer, and hopefully, eventually help them quit • DHS is particularly engaged in providing medication-assisted therapy (MAT) to all SUD patients who may benefit, this means prescribing buprenorphine to those with opiate use disorder (OUD) and naltrexone to those with alcohol use disorder • We generally advocate a “medication first” approach, meaning that a person does not need to be engaged in a broader treatment program in order to be offered MAT • If a patient comes in who is actively in opiate withdrawal, you can load them with buprenorphine during their UCC visit (up to 32 mg) using the protocol here • If a patient simply wants help quitting opiates and wants to try MAT, you can prescribe them buprenorphine to start at home once they start having withdrawal symptoms, and provide them the instructions on this handout • Numerous other resources for help treating OUD can be found here • UCSF Substance Use Warmline can be contacted for live access to help with difficult cases, Monday-Friday 6am-5pm: 855-300-3595 • If you do not have an x-waiver to prescribe buprenorphine yourself, we highly encourage getting your x-waiver, you can find training resources available here. We recommend the half and half in-person training as there are frequent sessions run by DHS staff. If there is interest in getting a group together for a training on site at Mid Valley, Rebecca Trotzky-Sirr (RTrotzky-Sirr@dhs.lacounty.gov) can be contacted who is the Director of the LAC+USC Urgent Care Clinic and is willing to conduct trainings on site when a group is interested. • Until you get your own x-waiver, you can draw on other urgent care clinic (UCC) staff to prescribe buprenorphine for you, as well as Dr. Jennifer Chen and Dr. Camilo Zaks from the primary care clinics who are willing to help • Substance Abuse Service (SASH) Helpline - to connect patients with a broader treatment program beyond MAT, the easiest way is to direct patients to call the SASH line at 1-844-804-7500. It is staffed 24/7 and the patient will speak to a counselor who will ask questions and help patient obtain services for detox and rehab.
Provider scheduling
• The provider schedule is available via www.amion.com • Type “LACamb midvalley” in the log in box to view the provider schedule • Emails will go out 2-3 months ahead of time requesting availability to make the providers schedule • You can view instructions on how to input your scheduling preferences into amion here • You can view instructions on advanced features of amion here like how to submit shift pick up requests or trades directly from amion or how to subscribe to a calendar feed of your shifts
Staff meetings
• Every morning there should be a huddle at 8 AM with providers, nursing, and reg staff to briefly check in and raise any anticipated issues for the day • Weekly, there is a pause in patient care for a 30-minute staff meeting at 3 PM on a rotating schedule of days of the week to include as many providers/staff as possible in announcements and discussion/troubleshooting of ongoing issues over time
Code assist
• Code assists are called when a patient appears to be in immediate distress (e.g. syncope, a fall, etc.) • The urgent care clinic responds to any code assist calls on the first floor • Clinic staff are not obligated to respond to call outside the building (e.g. in the parking lot, etc.) • Code assist calls on upper floors of MVCHC have staff on those floors that respond to them, however, when possible, the UCC should send a nursing representative to check in as some patients will be transferred to UCC for further eval after a code assist call
Social resources
• There are handouts for a variety of social resources created by Olive View Social Work that can be accessed here • Handouts available include shelter lists, food pantry lists, financial assistance lists, mental health resource lists, and information on getting welfare and food stamps • There are also several resources available on site for social needs o Medical-Legal Partnership (MLP) Clinic – Lawyers run a clinic at Mid Valley on the 5th floor Mondays and Tuesdays 8-4:30pm. Contact patient relations to make an appointment for your patient with the lawyers to address any kind of legal issue, including concerns around immigration status, eligibility for certain benefits, disputes with landlords, or family law issues. o Department of Public Social Services (DPSS) - Patients can be directed to DPSS in the Zev Yaroslavsky building next door to pursue financial and food assistance they may be eligible to receive o Safe Parking Program - Volunteers of America Greater Los Angeles (VOALA) operates a safe parking program for those residing in their cars out of the parking structure on the Mid Valley campus in the part of the parking structure adjacent to the Zev Yaroslavsky building from 9 PM to 6 AM each day. Patients can be directed to speak with staff on site in order to enroll in the safe parking program (if they are living in their vehicle and need a place to park overnight) or to connect with other services provided by VOALA for those experiencing homelessness. The contact for this program is Orland Ward at 213 251-7668. • There are also a few special programs to be aware of: o Los Angeles Homeless Outreach Program (LA-HOP) – If you meet a patient living on the streets, if you get from them where they can be found and/or a number they can be contacted at, you can fill out a LA-HOP referral here. It takes 30 seconds and set them up for a multidisciplinary street team (with experts on housing, mental health, substance abuse, and physical health) to follow up with the patient and get them connected with services they may be eligible for. o Countywide Benefits Entitlements Sevices Team (CBEST) - a program that helps people enroll in disability (meaning a patient can receive SSDI payments monthly as a disabled person) run by the county, you can view information on the program here. o Housing for Health (HFH) – a program that funds both interim and permanent supportive housing options for patients who are elderly or chronically ill suffering from homelessness. This program can get patients off the street in a matter of days and into interrim housing. The application takes a good 10 minutes to complete, but if you complete it and fax it in, the patient has a good chance of being rapidly housed in interim housing and eventually in permanent supportive housing. Application materials can be found here.
Continuing Care Clinic (CCC)
• CCC is a clinic within UCC at Mid Valley where patients can make return visits to the UCC • Under “follow up options” above it lays out all the different follow up options for a patient • CCC is meant to be used when a patient needs to see a physician face-to-face again in a short period of time and appointments with primary care are not available • CCC can also be used in cases where you are dealing with an acute issue that needs multiple visits in rapid succession, but will not need ongoing primary care management (e.g. bringing a patient back for a wound check, etc.) • The unit clerk, nursing, and PAC can all schedule the patient into a CCC appointment at your request • CCC appointments are available from 1 PM to 7:20 PM Monday to Friday • When a patient checks in for their CCC appointment, PAC staff cancels the actual appointment in PowerChart and then the patient is registered as if they are an urgent care patient in FirstNet • These patients can be seen just like any other urgent care patient by any provider working at the time, priority should be given to CCC patients arriving at their appointment time in getting the patient in a room when there is a backlog of other patients in the waiting room == Security == • Private security is available on site during all clinic hours • Security should be called for any behavioral emergency (Code Gold/Grey) to help restrain/contain the patient awaiting law enforcement (if necessary) • Security can also be called to help escort out patients refusing to leave the clinic or otherwise being disruptive • The contract with the private security company does allow them to place hands on the patients • Security is also available to walk staff to their cars on a limited basis when leaving after 11 PM • Security can be reached at • LA County Sheriff can also be called at X 73190 to escalate a situation
IT
• You can go to http://isd.lacounty.gov/reset-password/ to reset your password yourself and find IT resources/place a ticket • You can call the Enterprise Help Desk at 323-409-8000 for help with resetting your password and other IT problems • You can email the Enterprise Help Desk at helpdesk@dhs.lacounty.gov to create a ticket to fix an issue • There is local IT support during business hours available at
Feedback
• Patients can give feedback on their experience in the urgent care clinic (UCC) by pushing the happy or not button (and should be encouraged to do so) • Comment cards are also available for patients to leave comments/suggestions • Patients who want to share their (hopefully great) experience beyond the walls of Mid Valley can fill out a feedback form at http://dhs.lacounty.gov/wps/portal/dhs/feedback
MyWellness Online Patient Portal
• MyWellness is an online portal where patients can view a information on past and future visits, as well as all their medical test results, discharge instructions, and medications • Patients who are empaneled can even send appointment requests (and cancellations) through MyWellness • PAC staff can activate a MyWellness log in for a patient on request and they will receive an email inviting them to set up their log in • Patients can also set up their MyWellness log in on their own by going to http://dhs.lacounty.gov/wps/portal/dhs/mywellness/ or calling (877) 621-8014, but they will need their MRN to do so • There is a free smart phone app where patients can log in to view all their MyWellness portal information as well, it is called “HealtheLife” and can be searched in the Apple App store or Google Play store
Patient Eligibility/Insurance Status
• The MVCHC UCC is generally intended for “DHS eligible” patients. These are patients with Medi-cal managed care assigned to LA County DHS (e.g. LA Care assigned to DHS), patients with fee-for-service Medi-cal, patients with fee-for-service Medicare, and uninsured (“self-pay”) patients. • “Out-of-plan (OOP)” patients can be seen in the MVCHC UCC as well. These are patients who have Medi-cal managed care assigned to provider groups outside the county, commercially insured patients, or patients who do not reside in Los Angeles County. However, OOP patients are required to pay an $80 visit fee in order to be seen in the clinic. • Uninsured/self-pay patients will have to talk to patient relations after their visit in order to assess their eligibility for Medi-cal and other programs that may cover the costs of their care. If they are found to be eligible for these programs, their visit may be covered. If they are not eligible for any programs, they will be enrolled in the Ability-to-Pay (ATP) program. This program charges a fee on a sliding scale basis for the visit. In other words, if the patient is uninsured and high income, they may still need to pay the $80 fee. If they are low (or no) income, they may pay a reduced rate, or potentially no fee at all. • Any patient with questions about their financial status can visit patient relations on the 5th floor of MVCHC during business hours or call (818) 627-3000 and ask to speak to patient relations • For patients who have Medi-cal, but are assigned to a provider group outside the county, and would like to get their care in the county (and have regular access to our UCC) can talk to patient relations to get help switching their insurance assignment over to the county
Equipment/Supplies
• A full list of supplies stocked regularly in the UCC is available here o These supplies are all restocked by Olive View supply chain 1-2x per week, if you notice something is out (or near out) and not being restocked, you can contact Dan Raymond Rivera the head of OV supply chain at darivera@dhs.lacounty.gov, and please let nursing supervisors know as well • A full list of special order supplies for the UCC is available here o If you cannot find one of these items, use the last one, or realize it is close to running out, please inform nursing supervisors (Guadalupe or Berta) to let them know to put in an order to resupply these items • Special equipment available in the urgent includes o Slit lamp o Tonopen o Ring cutter o Wood’s lamp o Infant scale o Defibrillator/pacer o Portable suction o Bladder scanner o Accuvein o Broselow tape o Doppler


