Odontoid fracture
Background
- Also known as dens fracture
- Only stable if fracture confined to avulsion of the tip (superior to transverse ligament)[1]
- Bimodal distribution
- Young - blunt trauma to head, flexion/extension injury
- Elderly - fall, with higher morbidity/mortality
- False positives
- Dens and vertebral body are connected by cartilage at young age, and do not fuse until 3-6 yoa (up to 11 yoa)
- Os odontoideum - normal variant
Clinical Features
- Frequently involves other cervical spine injuries
- 25% associated with neurologic injury
Differential Diagnosis
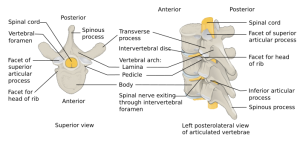
Vertebral fractures and dislocations types
- Cervical fractures and dislocations
- Thoracic and lumbar fractures and dislocations
Diagnosis
- Imaging
- Xray: AP, lateral, open-mouth odontoid view of cervical spine
- CT for further assessment if fracture identified
Types
- Type I: Oblique avulsion fracture of tip of odontoid; alar ligament avulsion
- Stable
- Atlanto-occipital instability (AAI) should be ruled out with flexion and extension films
- If AAI, requires surgical management
- Type II: Fracture at base of odontoid process where it attaches to C2; Fracture through waist
- Unstable
- high nonunion rate due to interruption of blood supply
- Young: Halo if no risk factors for nonunion, Surgery if risk factors for nonunion
- Elderly: Collar if not surgical candidates, Surgery if surgical candidates
- Type III: Extension of the fracture through upper portion of body of C2
- Unstable
Management
- Prehospital Immobilization see NAEMSP National Guidelines for Spinal Immobilization
- Consult ortho/neurosurgery/trauma
Disposition
See Also
References
- ↑ Clark, J., Abdullah, K. and Mroz, T. (2011) Biomechanics of the Craniovertebral Junction. Edited by Vaclav Klika