Cerebellar stroke: Difference between revisions
m (Rossdonaldson1 moved page Cerebellar Stroke to Cerebellar stroke) |
No edit summary |
||
| (18 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
==Background== | |||
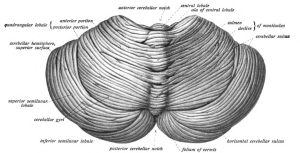
[[File:Gehirn, lateral - Lobi + Stammhirn + Cerebellum eng.svg|thumb|[[Sagital]] view of the brain.]] | |||
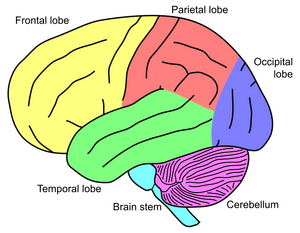
[[File:Sobo 1909 653.png|thumb|Superior/posterior view of the cerebellum.]] | |||
[[File:Circle of Willis en.png|thumb|Vascular anatomy of the Circle of Willis]] | |||
[[File:CerebellumArteries.jpg|thumb|The three major arteries of the cerebellum: the superior cerebellar artery (SCA), anterior inferior cerebellar artery(AICA), and the posterior inferior cerebellar artery (PICA).]] | |||
==Clinical Features== | ==Clinical Features== | ||
*Sudden inability to walk is common finding | *Sudden inability to walk is common finding | ||
*May have additional signs of of Posterior Circulation Stroke- 5Ds: Dizziness (Vertigo), Dysarthria, Dystaxia, Diplopia, Dysphagia | *May have additional signs of of Posterior Circulation Stroke- 5Ds: Dizziness ([[Vertigo]]), [[Dysarthria]], [[Dystaxia]], [[Diplopia]], [[Dysphagia]] | ||
*Can be confused | *Can be confused with acute vestibular syndrome (e.g. [[labyrinthitis]]) | ||
{{Central vs. peripheral causes of vertigo table}} | |||
==Differential Diagnosis== | |||
{{Vertigo DDX}} | |||
==Exam== | ==Evaluation== | ||
*[[EBQ:HINTS Exam|HINTS Exam]] | [[File:Leftsidedcerebellarstroke.png|thumb|Left sided cerebellar stroke due to occlusion of a vertebral artery.]] | ||
===Exam=== | |||
*[[EBQ:HINTS Exam|HINTS Exam]] | |||
{{Stroke workup}} | |||
== | ==Management== | ||
*Early neurosurgical consultation is needed (herniation may lead to rapid deterioration) | *Early neurosurgical consultation is needed (herniation may lead to rapid deterioration) | ||
*See [[Stroke (Main)]] | *See [[Stroke (Main)]] | ||
*See [[Thrombolysis in Acute Ischemic Stroke (tPA)]] | *See [[Thrombolysis in Acute Ischemic Stroke (tPA)]] | ||
==Disposition== | |||
*Admission | |||
==See Also== | ==See Also== | ||
*[[Stroke syndromes]] | *[[Stroke syndromes]] | ||
[[Category: | *[[Vertigo]] | ||
==External Links== | |||
[https://emcrit.org/emcrit/posterior-stroke/ EMCrit: Diagnosis of Posterior Stroke] | |||
==References== | |||
<references/> | |||
[[Category:Neurology]] | |||
Latest revision as of 23:05, 22 October 2025
Background
Sagital view of the brain.
Clinical Features
- Sudden inability to walk is common finding
- May have additional signs of of Posterior Circulation Stroke- 5Ds: Dizziness (Vertigo), Dysarthria, Dystaxia, Diplopia, Dysphagia
- Can be confused with acute vestibular syndrome (e.g. labyrinthitis)
Central vs. Peripheral Causes of Vertigo
| Peripheral | Central | |
| Onset | Sudden | Sudden or slow |
| Severity | Intense spinning | Ill defined, less intense |
| Pattern | Paroxysmal, intermittent | Constant |
| Aggravated by position/movement | Yes | Variable |
| Nausea/diaphoresis | Frequent | Variable |
| Nystagmus | Horizontal and unidirectional | Vertical and/or multidirectional |
| Fatigue of symptoms/signs | Yes | No |
| Hearing loss/tinnitus | May occur | Does not occur |
| Abnormal tympanic membrane | May occur | Does not occur |
| CNS symptoms/signs | Absent | Usually present |
Differential Diagnosis
Vertigo
- Vestibular/otologic
- Benign paroxysmal positional vertigo (BPPV)
- Traumatic (following head injury)
- Infection
- Ménière's disease
- Ear foreign body
- Otic barotrauma
- Otosclerosis
- Neurologic
- Cerebellar stroke
- Vertebrobasilar insufficiency
- Lateral Wallenberg syndrome
- Anterior inferior cerebellar artery syndrome
- Neoplastic: cerebellopontine angle tumors
- Basal ganglion diseases
- Vertebral Artery Dissection
- Multiple sclerosis
- Infections: neurosyphilis, tuberculosis
- Epilepsy
- Migraine (basilar)
- Other
- Hematologic: anemia, polycythemia, hyperviscosity syndrome
- Toxic
- Chronic renal failure
- Metabolic
Evaluation
Exam
Stroke Work-Up
- Labs
- POC glucose
- CBC
- Chemistry
- Coags
- Troponin
- T&S
- ECG
- In large ICH or stroke, may see deep TWI and prolong QT, occ ST changes
- Head CT (non-contrast)
- Also consider:
MR Imaging (for Rule-Out CVA or TIA)
- MRI Brain with DWI, ADC (without contrast) AND
- Cervical vascular imaging (ACEP Level B in patients with high short-term risk for stroke):[4]
- MRA brain (without contrast) AND
- MRA neck (without contrast)
- May instead use Carotid CTA or US (Carotid US slightly less sensitive than MRA)[5] (ACEP Level C)
Management
- Early neurosurgical consultation is needed (herniation may lead to rapid deterioration)
- See Stroke (Main)
- See Thrombolysis in Acute Ischemic Stroke (tPA)
Disposition
- Admission
See Also
External Links
EMCrit: Diagnosis of Posterior Stroke
References
- ↑ Mullins ME, Schaefer PW, Sorensen AG, Halpern EF, Ay H, He J, Koroshetz WJ, Gonzalez RG. CT and conventional and diffusion-weighted MR imaging in acute stroke: study in 691 patients at presentation to the emergency department. Radiology. 2002 Aug;224(2):353-60.
- ↑ Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006; 354(4):387–396.
- ↑ Douglas VC, Johnston CM, Elkins J, et al. Head computed tomography findings predict short-term stroke risk after transient ischemic attack. Stroke. 2003;34:2894-2899.
- ↑ ACEP Clinical Policy: Suspected Transient Ischemic Attack full text
- ↑ Nederkoorn PJ, Mali WP, Eikelboom BC, et al. Preoperative diagnosis of carotid artery stenosis. Accuracy of noninvasive testing. Stroke. 2002;33:2003-2008.