Splenic trauma: Difference between revisions
| (18 intermediate revisions by 6 users not shown) | |||
| Line 4: | Line 4: | ||
==Clinical Features== | ==Clinical Features== | ||
*[[LUQ pain]] | *[[LUQ pain]] | ||
*Signs of shock | *Signs of [[shock]] | ||
*[[Hypotension]] | *[[Hypotension]] | ||
*Left lower rib pain | *Left lower [[chest wall pain|rib pain]] | ||
*Kehr's sign | *Kehr's sign | ||
**Acute pain in the tip of the shoulder due to the presence of blood in the peritoneal cavity when a patient's legs are elevated while laying flat. | **Acute pain in the tip of the shoulder due to the presence of blood in the peritoneal cavity when a patient's legs are elevated while laying flat. | ||
| Line 13: | Line 13: | ||
{{Abdominal trauma DDX}} | {{Abdominal trauma DDX}} | ||
== | ==Evaluation== | ||
[[File:Milzruptur - Computertomographie axial - pv-Kontrastphase 001.jpg|thumb|Traumatic rupture of the spleen on contrast enhanced axial CT (portal venous phase).]] | |||
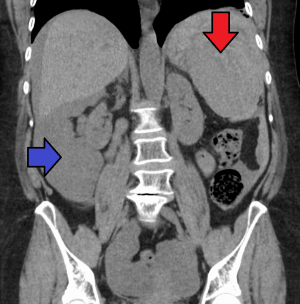
[[File:SpleenHematomaAndBloodAbdoCor.png|thumb|Splenic hematoma (red arrow) resulting in free abdominal blood (blue arrow).]] | |||
{{ATLS abd trauma diagnosis algorithm}} | {{ATLS abd trauma diagnosis algorithm}} | ||
| Line 22: | Line 24: | ||
| align="center" style="background:#f0f0f0;"|'''Laceration''' | | align="center" style="background:#f0f0f0;"|'''Laceration''' | ||
|- | |- | ||
| I||Subcapsular, <10% of surface area||Capsular tear <1 cm in depth into the parenchyma | | I|| | ||
*Subcapsular, <10% of surface area | |||
|| | |||
*Capsular tear <1 cm in depth into the parenchyma | |||
|- | |- | ||
| II||Subcapsular, 10-50% of surface area||Capsular tear, 1 to 3 cm in depth, but not involving a trabecular vessel | | II|| | ||
*Subcapsular, 10-50% of surface area | |||
|| | |||
*Capsular tear, 1 to 3 cm in depth, but not involving a trabecular vessel | |||
|- | |- | ||
| III||Subcapsular, >50% of surface area OR expanding, | | III|| | ||
*Subcapsular, >50% of surface area OR expanding, | |||
*Ruptured subcapsular or parenchymal hematoma | |||
*OR, intraparenchymal hematoma >5 cm or expanding | |||
OR intraparenchymal hematoma >5 cm or expanding | || | ||
|| | *Capsular tear, 3 to 10 cm in depth or involving a trabecular vessel. | ||
|- | |- | ||
| IV||||Involving segmental or hilar vessels with major devascularization (i.e. >25% of spleen) | | IV||| | ||
*Subcapsular or central hematoma > 10cm | |||
|| | |||
*Involving segmental or hilar vessels with major devascularization (i.e. >25% of spleen) | |||
|- | |- | ||
| V||Shattered spleen||Hilar vascular injury which devascularizes spleen. | | V|| | ||
*Shattered spleen | |||
|| | |||
*Hilar vascular injury which devascularizes spleen. | |||
|} | |} | ||
Interactive calculators have been developed that facilitate grading of splenic injuries per AAST guidelines.<ref> [https://radathand.com/radiology-calculators/emergency-radiology-calculator/spleen-trauma-injury-score-aast/ Spleen trauma injury score calculator]- ''Rad At Hand'' </ref> | |||
==Management== | ==Management== | ||
| Line 42: | Line 57: | ||
**Hemodynamic status of the patient | **Hemodynamic status of the patient | ||
**Grade of splenic injury | **Grade of splenic injury | ||
**Presence of other injuries and medical comorbidities | **Presence of other injuries and medical comorbidities | ||
*Operative Management | |||
**Indicated for diffuse peritonitis or hemodynamic instability after blunt abdominal trauma | |||
**Not indicated based on injury grade alone<ref>Stassen N, Bhullar I, Cheng J, et al. Selective nonoperative management of blunt splenic injury: An Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg 2012; 73(5):s293-s300</ref> | |||
*Nonoperative management | *Nonoperative management | ||
**Failure rate of 10-15% | **Failure rate of 10-15% | ||
**Some advocate nonoperative management only if <55yr and CT injury grade less than IV | **Some advocate nonoperative management only if <55yr and CT injury grade less than IV | ||
**Should only be considered in locations with resources available for urgent laparotomy | |||
==Disposition== | ==Disposition== | ||
*Admit | |||
==See Also== | ==See Also== | ||
| Line 54: | Line 74: | ||
==References== | ==References== | ||
<References/> | <References/> | ||
[[Category:Trauma]] | [[Category:Trauma]] | ||
Latest revision as of 23:20, 18 July 2024
Background
- Most commonly injured visceral organ in blunt trauma
Clinical Features
- LUQ pain
- Signs of shock
- Hypotension
- Left lower rib pain
- Kehr's sign
- Acute pain in the tip of the shoulder due to the presence of blood in the peritoneal cavity when a patient's legs are elevated while laying flat.
Differential Diagnosis
Abdominal Trauma
- Abdominal compartment syndrome
- Diaphragmatic trauma
- Duodenal hematoma
- Genitourinary trauma
- Liver trauma
- Pelvic fractures
- Retroperitoneal hemorrhage
- Renal trauma
- Splenic trauma
- Trauma in pregnancy
- Ureter trauma
Evaluation
ATLS Blunt Abdominal Trauma Algorithm
- Unstable
- Stable
- CT scan
- Exploratory laparotomy, angiographic embolization, conservative management as indicated
- CT scan
AAST Criteria
| Grade | Hematoma | Laceration |
| I |
|
|
| II |
|
|
| III |
|
|
| IV |
|
|
| V |
|
|
Interactive calculators have been developed that facilitate grading of splenic injuries per AAST guidelines.[1]
Management
- Observation, angiographic embolization, or surgery depending upon:
- Hemodynamic status of the patient
- Grade of splenic injury
- Presence of other injuries and medical comorbidities
- Operative Management
- Indicated for diffuse peritonitis or hemodynamic instability after blunt abdominal trauma
- Not indicated based on injury grade alone[2]
- Nonoperative management
- Failure rate of 10-15%
- Some advocate nonoperative management only if <55yr and CT injury grade less than IV
- Should only be considered in locations with resources available for urgent laparotomy
Disposition
- Admit
See Also
References
- ↑ Spleen trauma injury score calculator- Rad At Hand
- ↑ Stassen N, Bhullar I, Cheng J, et al. Selective nonoperative management of blunt splenic injury: An Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg 2012; 73(5):s293-s300