Skin abscess: Difference between revisions
| Line 30: | Line 30: | ||
**Abscess in an immunocompromised or diabetic patient | **Abscess in an immunocompromised or diabetic patient | ||
*[[Antibiotics]] | *[[Antibiotics]] | ||
** | **Although withholding antibiotics is part of [[Choosing wisely ACEP]], new evidence suggest antibiotic NNT of 14 to prevent 1 treatment failure<ref>Talan DA, et al. Trimethoprim–Sulfamethoxazole versus placebo for uncomplicated skin abscess. NEJM. 2016; 374(9):823-832.</ref> | ||
**[[TMP/SMX]] x 5 days (all abscesses)<ref>[[EBQ:TMP-SMX vs Placebo for Uncomplicated Skin Abscess]]</ref> | **[[TMP/SMX]] x 5 days (all abscesses)<ref>[[EBQ:TMP-SMX vs Placebo for Uncomplicated Skin Abscess]]</ref> | ||
**Consider more aggressive antibiotic treatment if concomitant [[cellulitis]] | **Consider more aggressive antibiotic treatment if concomitant [[cellulitis]] | ||
Revision as of 16:45, 23 January 2017
Background
Clinical Features
- Tender nodular region with surrounding induration
- Fluctuance
- Surrounding erythema
Differential Diagnosis
- Cyst
- Vascular malformation
Skin and Soft Tissue Infection
- Cellulitis
- Erysipelas
- Lymphangitis
- Folliculitis
- Hidradenitis suppurativa
- Skin abscess
- Necrotizing soft tissue infections
- Mycobacterium marinum
Look-A-Likes
- Sporotrichosis
- Osteomyelitis
- Deep venous thrombosis
- Pyomyositis
- Purple glove syndrome
- Tuberculosis (tuberculous inflammation of the skin)
Evaluation
- Clinical exam
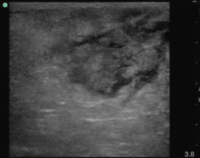
- Soft tissue ultrasound can differentiate between abscess and cellulitis
- Assess for fluid collection and swirl within the collection
Management
- Incision and drainage
- Packing
- Abscess >5 cm in diameter
- Pilonidal abscess
- Abscess in an immunocompromised or diabetic patient
- Antibiotics
- Although withholding antibiotics is part of Choosing wisely ACEP, new evidence suggest antibiotic NNT of 14 to prevent 1 treatment failure[4]
- TMP/SMX x 5 days (all abscesses)[5]
- Consider more aggressive antibiotic treatment if concomitant cellulitis
Disposition
- Admission - Reserved for significantly ill patients or those requiring surgical intervention
- Discharge – Appropriate for majority of patients
- Follow up in 2 days for wound check
See Also
External Links
- EMNerd Case of the Pragmatic Wound
- Are Antibiotics Back in Favor for Abscesses?
- Sonoguide: Abscess Assessment
References
- ↑ Maligner D et al. The prevalence of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) in skin abscesses presenting to the pediatric emergency department. N C Med J. 2008 Sep-Oct;69(5):351-4.
- ↑ Pickett A et al. Changing incidence of methicillin-resistant staphylococcus aureus skin abscesses in a pediatric emergency department. Pediatr Emerg Care. 2009 Dec;25(12):831-4.
- ↑ Bradley W. Frazee et al. High Prevalence of Methicillin-Resistant Staphylococcus aureus in Emergency Department Skin and Soft Tissue Infections http://dx.doi.org/10.1016/j.annemergmed.2004.10.011
- ↑ Talan DA, et al. Trimethoprim–Sulfamethoxazole versus placebo for uncomplicated skin abscess. NEJM. 2016; 374(9):823-832.
- ↑ EBQ:TMP-SMX vs Placebo for Uncomplicated Skin Abscess