Deterioration after intubation: Difference between revisions
No edit summary |
|||
| (17 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
==Background== | ==Background== | ||
*There are multiple reasons for a patient to deteriorate while on mechanical ventilation | |||
*A systematic method of evaluating this deterioration is the best way to identify/fix the causative problem | |||
==Clinical Features== | ==Clinical Features== | ||
*Desaturation, other vital sign abnormalities, or | *Desaturation, other vital sign abnormalities, or [[cardiac arrest]] while on mechanical ventilation | ||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
=== | ===DOPES<ref>EMRA Critical Care Handbook</ref><ref>Monica E. Kleinman et al. Pediatric Advanced Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. AAP. 2010. http://pediatrics.aappublications.org/content/126/5/e1361.full</ref>=== | ||
*'''D'''isplaced ETT | *'''D'''isplaced ETT | ||
*'''O'''bstruction (anywhere along circuit) | *'''O'''bstruction (anywhere along circuit) | ||
*[[Pneumothorax|'''P'''neumothorax]] | *[[Pneumothorax|'''P'''neumothorax]] | ||
*'''E'''quipment failure (ventilator malfunction or disconnect) | *'''E'''quipment failure (ventilator malfunction or disconnect) | ||
*'''S'''tacked breaths (asthmatics) | |||
== | ==Evaluation== | ||
*Clinical | *Clinical | ||
| Line 17: | Line 20: | ||
===Troubleshoot=== | ===Troubleshoot=== | ||
''Immediately disconnect from ventilator (allows for expiration of stacked breaths)'' | ''Immediately disconnect from ventilator (allows for expiration of stacked breaths)'' | ||
*D - Displacement of tube | *D - Displacement of tube or cuff | ||
**Attach end-tidal CO2 to verify and check depth (cm at lip) | **Attach end-tidal CO2 to verify and check depth (cm at lip) | ||
*O - Obstruction of tube/circuit | *O - Obstruction of tube/circuit | ||
**Use suction catheter to remove mucus plug, or make sure | **Use suction catheter to remove mucus plug, or make sure patient not biting down, look for kink in tube | ||
*P - Pneumothorax | *P - [[Pneumothorax]] | ||
**Verify via [[Ultrasound: Lungs|ultrasound]], CXR, or [[needle thoracostomy]] (high suspicion) | **Verify via [[Ultrasound: Lungs|ultrasound]], CXR, or [[needle thoracostomy]] (high suspicion) | ||
*E - Equipment failure | *E - Equipment failure | ||
| Line 29: | Line 32: | ||
===Fix=== | ===Fix=== | ||
*Disconnect | *"DOTTS" Mnemonic | ||
*Oxygen 100% | *D - Disconnect ventilator and put light pressure on patient chest | ||
*O - Oxygen 100% BVM. Look for chest rise, listen and feel for cuff leak | |||
*Tube | *T - Tube position and patency. Pass bougie or suction all the way through tube to remove obstruction | ||
*T - Tweak the vent. Usually need to decrease respiratory rate, decreased inspiratory time with changing E:I ratio (see below on breath-staking) | |||
*Tweak | *S - Sonography and CXR | ||
*Sonography | |||
===Auto-PEEP (Breath stacking) troubleshooting options=== | ===Auto-PEEP (Breath stacking) troubleshooting options=== | ||
| Line 46: | Line 46: | ||
*Decrease TV | *Decrease TV | ||
*Increase sedation | *Increase sedation | ||
===Peak Vs Plateau Pressure=== | |||
*Super important to keep alveolar pressure low to prevent barotrauma | |||
*Peak Pressure is pressure of entire system (vent, ET tube, trachea, bronchus, bronchioles, alveoli). High peak pressure does not equal barotrauma | |||
*Plateau pressure - check with button on vent (may say plateau pressure or end-inspiratory hold) | |||
*High Peak and Normal Plateau - problem with vent, ET tube, bronchoconstriction (reactive airway disease/asthma/COPD). | |||
*High Peak and High Plateau - Compliance issue (pneumothorax, problem with alveoli like ARDS, fluid overload). Need to decrease pressure to prevent barotrauma. | |||
*Plateau pressures should be kept < 30mmHg if possible. | |||
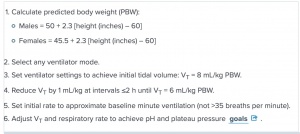
[[File:ardsnet.jpg|thumb|[http://www.ardsnet.org/files/ventilator_protocol_2008-07.pdf ARDS net ventilator protocol ]]] | |||
{{Lung Protective FiO2 and PEEP Scale}} | |||
==See Also== | ==See Also== | ||
{{Mechanical ventilation pages}} | {{Mechanical ventilation pages}} | ||
{{Related Difficult Airway Pages}} | |||
==External Links== | |||
*https://rebelem.com/rebel-cast-ep-46b-vent-management-crashing-patient-haney-mallemat/ | |||
==References== | ==References== | ||
<references/> | <references/> | ||
[[Category: | [[Category:Pulmonary]] | ||
[[Category:Critical Care]] | [[Category:Critical Care]] | ||
Latest revision as of 16:10, 24 April 2024
Background
- There are multiple reasons for a patient to deteriorate while on mechanical ventilation
- A systematic method of evaluating this deterioration is the best way to identify/fix the causative problem
Clinical Features
- Desaturation, other vital sign abnormalities, or cardiac arrest while on mechanical ventilation
Differential Diagnosis
DOPES[1][2]
- Displaced ETT
- Obstruction (anywhere along circuit)
- Pneumothorax
- Equipment failure (ventilator malfunction or disconnect)
- Stacked breaths (asthmatics)
Evaluation
- Clinical
Management
Troubleshoot
Immediately disconnect from ventilator (allows for expiration of stacked breaths)
- D - Displacement of tube or cuff
- Attach end-tidal CO2 to verify and check depth (cm at lip)
- O - Obstruction of tube/circuit
- Use suction catheter to remove mucus plug, or make sure patient not biting down, look for kink in tube
- P - Pneumothorax
- Verify via ultrasound, CXR, or needle thoracostomy (high suspicion)
- E - Equipment failure
- Connect to BVM
- S - Stacked breaths - Auto-PEEP especially in COPD/Asthma
- Disconnect from ventilator
Fix
- "DOTTS" Mnemonic
- D - Disconnect ventilator and put light pressure on patient chest
- O - Oxygen 100% BVM. Look for chest rise, listen and feel for cuff leak
- T - Tube position and patency. Pass bougie or suction all the way through tube to remove obstruction
- T - Tweak the vent. Usually need to decrease respiratory rate, decreased inspiratory time with changing E:I ratio (see below on breath-staking)
- S - Sonography and CXR
Auto-PEEP (Breath stacking) troubleshooting options
- Bronchodilators if COPD/asthma
- Decrease RR
- Decrease I:E ratio (increase expiratory time)
- Quicker inspiratory flow rate
- Decrease TV
- Increase sedation
Peak Vs Plateau Pressure
- Super important to keep alveolar pressure low to prevent barotrauma
- Peak Pressure is pressure of entire system (vent, ET tube, trachea, bronchus, bronchioles, alveoli). High peak pressure does not equal barotrauma
- Plateau pressure - check with button on vent (may say plateau pressure or end-inspiratory hold)
- High Peak and Normal Plateau - problem with vent, ET tube, bronchoconstriction (reactive airway disease/asthma/COPD).
- High Peak and High Plateau - Compliance issue (pneumothorax, problem with alveoli like ARDS, fluid overload). Need to decrease pressure to prevent barotrauma.
- Plateau pressures should be kept < 30mmHg if possible.
Lung Protective FiO2 and PEEP Scale[3][4][5]
| FiO2 | 0.3 | 0.4 | 0.4 | 0.5 | 0.5 | 0.6 | 0.7 | 0.7 | 0.7 | 0.8 | 0.9 | 0.9 | 0.9 | 1.0 | 1.0 | 1.0 |
| PEEP | 5 | 5 | 8 | 8 | 10 | 10 | 10 | 12 | 14 | 14 | 14 | 16 | 18 | 20 | 22 | 24 |
See Also
Mechanical Ventilation Pages
- Noninvasive ventilation
- Intubation
- Mechanical ventilation (main)
- Miscellaneous
Airway Pages
- Pre-intubation
- Induction
- Intubation
- Surgical airways
- Post-intubation
External Links
References
- ↑ EMRA Critical Care Handbook
- ↑ Monica E. Kleinman et al. Pediatric Advanced Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. AAP. 2010. http://pediatrics.aappublications.org/content/126/5/e1361.full
- ↑ The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342(18):1301-1308.
- ↑ Kallet RH, et al. "Respiratory controversies in the critical care setting. Do the NIH ARDS Clinical Trials Network PEEP/FIO2 tables provide the best evidence-based guide to balancing PEEP and FIO2 settings in adults?" Respiratory Care. 2007. 52(4):461-75.
- ↑ ARDSnet protocol card