Lower back pain: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
==Background== | ==Background== | ||
*Pain lasting >6wks is risk factor for more serious disease | *Pain lasting >6wks is risk factor for more serious disease | ||
*Night pain and unrelenting pain are worrisome symptoms | |||
*Back pain in IV drug user is spinal infection until proven otherwise | *Back pain in IV drug user is spinal infection until proven otherwise | ||
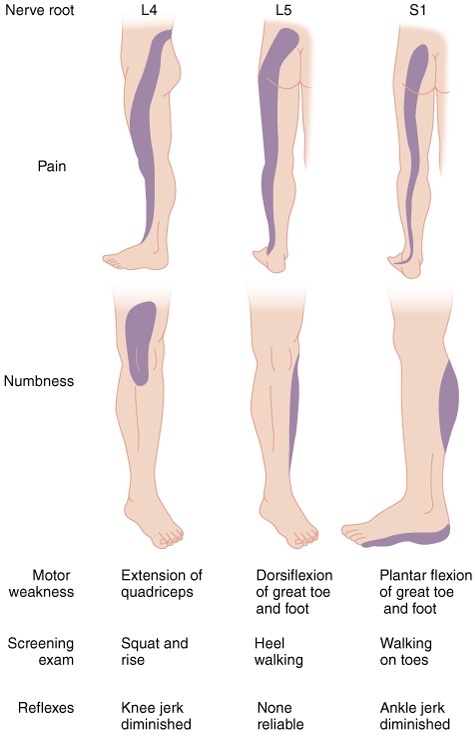
* | *95% of herniated discks occur at L4-L5 or L5-S1 (for both pain extends below the knee) | ||
==Clinical Features== | ==Clinical Features== | ||
| Line 10: | Line 11: | ||
**Pain worse w/ movement but improves w/ rest | **Pain worse w/ movement but improves w/ rest | ||
*Spinal stenosis | *Spinal stenosis | ||
**Bilateral sciatic pain worsened by walking, prolonged standing | **Bilateral sciatic pain worsened by walking (pseudoclaudication), prolonged standing **Pain relieved by forward flexion | ||
*Sciatica | *Sciatica | ||
** | **Radicular back pain in the distribution of a lumbar or sacral nerve root | ||
***Anything that compresses the nerve roots, cauda equina, or cord can cause sciatica | |||
**Pain worsened by coughing, Valsalva, sitting; relieved by lying in supine position | **Pain worsened by coughing, Valsalva, sitting; relieved by lying in supine position | ||
**Occurs in only 1% of pts w/ back pain | **Occurs in only 1% of pts w/ back pain | ||
**95% of herniated | **Present in 95% of pts who have a symptomatic herniated disk | ||
[[File:Lumbar_Nerve_Root_Compromise.jpg]] | [[File:Lumbar_Nerve_Root_Compromise.jpg]] | ||
| Line 31: | Line 33: | ||
###Lifting the asymptomatic leg causes radicular pain down the affected leg | ###Lifting the asymptomatic leg causes radicular pain down the affected leg | ||
##Nerve root compromise | ##Nerve root compromise | ||
# | ##Rectal exam (if concerned for cord compression) | ||
#Labs | #Labs | ||
##CBC | ##Only necessary if concerned for infection, tumor, or rheumatologic cause | ||
# | ###CBC, UA, ESR (90-98% Sn for infectious etiology) | ||
## | #Imaging | ||
#### | ##Plain films | ||
#### | ###Only necessary if suspect fracture, tumor, or infection | ||
# | ##MRI | ||
# | ###Only necessary if suspect infection, neoplasm, epidural compression syndromes | ||
#US | ###Consider for back pain >6-8wks | ||
##Rule-out AAA | ##US | ||
###Rule-out AAA | |||
==Treatment== | |||
*Nonspecific Back Pain (musculoskeletal) | |||
**Instruct to continue daily activities using pain as limiting factor | |||
**Meds | |||
***NSAIDs or acetaminophen | |||
****1st line therapy | |||
***Opioids | |||
****Appropriate for moderate-severe pain but only for limited duration (1-2wks) | |||
***Muscle relaxants | |||
****Efficacy appears equal to NSAIDs | |||
****Diazepam 5-10mg PO q6-8hr OR methocarbamol 1000-1500mg PO QID | |||
*Sciatica | |||
**Treatment is the same as for musculoskeletal back pain | |||
**80% of pts will ultimately improve without surgery | |||
*Spinal Stenosis | |||
**Treatment is the same as for musculoskeletal back pain | |||
== See Also == | == See Also == | ||
*[[Back Pain (Red Flags)]] | *[[Back Pain (Red Flags)]] | ||
* | *[[Back Pain (DDX)]] | ||
== Source == | == Source == | ||
Revision as of 05:53, 19 February 2012
Background
- Pain lasting >6wks is risk factor for more serious disease
- Night pain and unrelenting pain are worrisome symptoms
- Back pain in IV drug user is spinal infection until proven otherwise
- 95% of herniated discks occur at L4-L5 or L5-S1 (for both pain extends below the knee)
Clinical Features
- See Back Pain (Red Flags)
- Musculoskeletal pain
- Located primarily in the back w/ possible radiation into the buttock/thighs
- Pain worse w/ movement but improves w/ rest
- Spinal stenosis
- Bilateral sciatic pain worsened by walking (pseudoclaudication), prolonged standing **Pain relieved by forward flexion
- Sciatica
- Radicular back pain in the distribution of a lumbar or sacral nerve root
- Anything that compresses the nerve roots, cauda equina, or cord can cause sciatica
- Pain worsened by coughing, Valsalva, sitting; relieved by lying in supine position
- Occurs in only 1% of pts w/ back pain
- Present in 95% of pts who have a symptomatic herniated disk
- Radicular back pain in the distribution of a lumbar or sacral nerve root
DDX
- See Back Pain (DDX)
Work-Up
- Pregnancy test
- Exam
- Straight leg raise testing
- Screening exam for a herniated disk (Sn 68-80%)
- Lifting leg causes radicular pain of affected leg radiating to BELOW the knee
- Pain is worsened by ankle dorsiflexion
- Crossed Straight leg raise testing (high Sp, low Sn)
- Lifting the asymptomatic leg causes radicular pain down the affected leg
- Nerve root compromise
- Rectal exam (if concerned for cord compression)
- Straight leg raise testing
- Labs
- Only necessary if concerned for infection, tumor, or rheumatologic cause
- CBC, UA, ESR (90-98% Sn for infectious etiology)
- Only necessary if concerned for infection, tumor, or rheumatologic cause
- Imaging
- Plain films
- Only necessary if suspect fracture, tumor, or infection
- MRI
- Only necessary if suspect infection, neoplasm, epidural compression syndromes
- Consider for back pain >6-8wks
- US
- Rule-out AAA
- Plain films
Treatment
- Nonspecific Back Pain (musculoskeletal)
- Instruct to continue daily activities using pain as limiting factor
- Meds
- NSAIDs or acetaminophen
- 1st line therapy
- Opioids
- Appropriate for moderate-severe pain but only for limited duration (1-2wks)
- Muscle relaxants
- Efficacy appears equal to NSAIDs
- Diazepam 5-10mg PO q6-8hr OR methocarbamol 1000-1500mg PO QID
- NSAIDs or acetaminophen
- Sciatica
- Treatment is the same as for musculoskeletal back pain
- 80% of pts will ultimately improve without surgery
- Spinal Stenosis
- Treatment is the same as for musculoskeletal back pain
See Also
Source
- Tintinalli