Burr hole: Difference between revisions
No edit summary |
(extensive additions) |
||
| Line 1: | Line 1: | ||
==Indications== | ==Indications== | ||
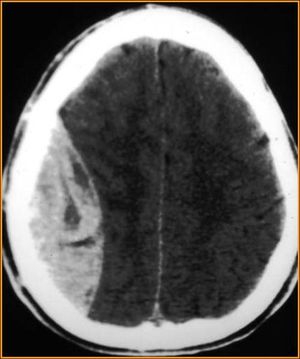
Rapidly deteriorating patients (GCS < 8) with imaging evidence of epidural hematoma causing midline shift, unequal pupils, for whom timely intervention by neurosurgery is not possible. Every attempt should be made to discuss the patient and plan for procedure with a neurosurgeon prior to intervention. | |||
[[File:Epidural_Hematoma.jpg|thumb|Epidural hematoma without significant midline shift]] | |||
==Contraindications== | ==Contraindications== | ||
*GCS >8 | *GCS > 8 | ||
* | *No neuroimaging | ||
* | *Neurosurgical intervention available within a timely manner | ||
==Equipment Needed== | ==Equipment Needed== | ||
Many items contained in pre-packaged Cranial Access Kit | |||
*Knife | |||
* | *Self-retaining retractor | ||
* | *Drill | ||
*Bipolar cautery (if available* | |||
*Drill | |||
* | |||
* | |||
==Procedure<ref | ==Procedure<ref>Wilson MH, Wise D, Davies G, Lockey D. Emergency burr holes: "How to do it". Scand J Trauma Resusc Emerg Med. 2012; 20: 24.== | ||
* | *Do not delay transfer if timely neurosurgical intervention is available | ||
* | *Medically optimize the patient (intubated, normotensive, c-spine precautions, +/- mannitol or hypertonic saline in consultation with a neurosurgeon) | ||
* | *Place the patient in the supine position | ||
** | *Ensure indications are appropriate. | ||
* | *Review position of the hematoma on Head CT | ||
*Using a marking pen, mark a 3cm line for the incision | |||
*Cleanse | *Cleanse the area appropriately (chlorhexidine/betadine) | ||
* | *Drape in sterile fashion | ||
* | *Using knife, make a small incision down to the bone | ||
* | **Control bleeding with direct pressure | ||
* | *Using a knife, push the periosteum aside | ||
** | *Insert a self-retaining retractor | ||
* | *Use hand drill with firm pressure, surface of drill bit parallel to bone surface (drill perpendicular to bone) | ||
* | **If available, have an assistant hold the head still from beneath the drape | ||
* | **Also consider an additional assistant applying sterile saline to the drill site while creating burr hole | ||
* | *Slow drill speed once at the inner table of the skull; remove drill | ||
* | *Remove any remaining bony fragments | ||
*Drain visible (flowing) extradural blood | |||
*Subdural blood may be evacuated following dural puncture (do not perform unless trained and neurosurgical consultant advises) | |||
* | **This is technically more difficult, as subdural blood is more likely to clot and be difficult to evauate | ||
*Transfer patient to facility with neurosurgical capabilities | |||
==Complications== | ==Complications== | ||
* | *Procedure failure (incorrect position, equipment malfunction, etc.) | ||
*Damage to brain parenchyma | *Damage to brain parenchyma | ||
*Intracranial infection | |||
*Damage to subdural contents | |||
*Continued bleeding | |||
==See Also== | ==See Also== | ||
[[Epidural hemorrhage]] | [[Epidural hemorrhage]] | ||
[ | |||
==External Links== | |||
[http://resus.me/burr-holes-by-emergency-physicians/ Resus.Me Discussion of Burr Holes by Emergency Physicians] | |||
==References== | ==References== | ||
*Smith SW, Clark M, Nelson J, Heegaard W, Lufkin KC, Ruiz E. Emergency department skull trephination for epidural hematoma in patients who are awake but deteriorate rapidly. J Emerg Med. 2010 Sep;39(3):377-83. doi: 10.1016/j.jemermed.2009.04.062. Epub 2009 Jun 17. | |||
<references/> | <references/> | ||
Revision as of 21:29, 17 August 2015
Indications
Rapidly deteriorating patients (GCS < 8) with imaging evidence of epidural hematoma causing midline shift, unequal pupils, for whom timely intervention by neurosurgery is not possible. Every attempt should be made to discuss the patient and plan for procedure with a neurosurgeon prior to intervention.
Contraindications
- GCS > 8
- No neuroimaging
- Neurosurgical intervention available within a timely manner
Equipment Needed
Many items contained in pre-packaged Cranial Access Kit
- Knife
- Self-retaining retractor
- Drill
- Bipolar cautery (if available*
Procedure<ref>Wilson MH, Wise D, Davies G, Lockey D. Emergency burr holes: "How to do it". Scand J Trauma Resusc Emerg Med. 2012; 20: 24.
- Do not delay transfer if timely neurosurgical intervention is available
- Medically optimize the patient (intubated, normotensive, c-spine precautions, +/- mannitol or hypertonic saline in consultation with a neurosurgeon)
- Place the patient in the supine position
- Ensure indications are appropriate.
- Review position of the hematoma on Head CT
- Using a marking pen, mark a 3cm line for the incision
- Cleanse the area appropriately (chlorhexidine/betadine)
- Drape in sterile fashion
- Using knife, make a small incision down to the bone
- Control bleeding with direct pressure
- Using a knife, push the periosteum aside
- Insert a self-retaining retractor
- Use hand drill with firm pressure, surface of drill bit parallel to bone surface (drill perpendicular to bone)
- If available, have an assistant hold the head still from beneath the drape
- Also consider an additional assistant applying sterile saline to the drill site while creating burr hole
- Slow drill speed once at the inner table of the skull; remove drill
- Remove any remaining bony fragments
- Drain visible (flowing) extradural blood
- Subdural blood may be evacuated following dural puncture (do not perform unless trained and neurosurgical consultant advises)
- This is technically more difficult, as subdural blood is more likely to clot and be difficult to evauate
- Transfer patient to facility with neurosurgical capabilities
Complications
- Procedure failure (incorrect position, equipment malfunction, etc.)
- Damage to brain parenchyma
- Intracranial infection
- Damage to subdural contents
- Continued bleeding
See Also
External Links
Resus.Me Discussion of Burr Holes by Emergency Physicians
References
- Smith SW, Clark M, Nelson J, Heegaard W, Lufkin KC, Ruiz E. Emergency department skull trephination for epidural hematoma in patients who are awake but deteriorate rapidly. J Emerg Med. 2010 Sep;39(3):377-83. doi: 10.1016/j.jemermed.2009.04.062. Epub 2009 Jun 17.